Anemia Pada Pasien Ginjal Kronik, Bagaimana Dampak Dan Pengobatannya?
Summary
TLDRThis webinar delves into the causes, impact, and management of anemia in chronic kidney disease (CKD). It explains how anemia develops due to erythropoietin deficiency, iron imbalance, and shortened red blood cell lifespan. The presentation outlines the clinical consequences, including fatigue, cardiovascular strain, and reduced quality of life. Treatment strategies include erythropoiesis-stimulating agents (ESAs), iron supplementation, and blood transfusions, with a focus on tailored approaches for each patient. The webinar emphasizes the importance of correcting iron deficiency before initiating ESA therapy and regularly monitoring patient response to improve outcomes.
Takeaways
- 😀 Anemia in chronic kidney disease (CKD) increases in severity as the disease progresses, reaching over 50% in stage 4 and stage 5 CKD patients.
- 😀 According to KDIGO 2012, anemia is defined by hemoglobin (Hb) levels below 13 g/dL for men and below 12 g/dL for women.
- 😀 Anemia in CKD is commonly due to erythropoietin (EPO) deficiency, shortened red blood cell lifespan, and iron deficiency, among other factors.
- 😀 Iron metabolism is disrupted in CKD, with elevated hepcidin levels causing decreased iron absorption and use, exacerbating anemia.
- 😀 Erythropoiesis depends not only on EPO but also on sufficient iron and proper nutrition for the production of red blood cells.
- 😀 Chronic inflammation, common in CKD, increases hepcidin production, leading to iron sequestration and worsened anemia.
- 😀 Anemia leads to hypoxia, which increases the workload on the heart, potentially leading to heart failure in CKD patients.
- 😀 Symptoms of anemia include fatigue, dizziness, shortness of breath on light exertion, and palpitations, all of which decrease quality of life.
- 😀 CKD-related anemia is managed by correcting iron deficiency, administering erythropoiesis-stimulating agents (ESA), and addressing underlying conditions like secondary hyperparathyroidism and inflammation.
- 😀 Transfusion is not the first-line treatment for anemia in CKD and is reserved for extreme cases with severe symptoms or hemoglobin levels below 7 g/dL.
Q & A
What is anemia in chronic kidney disease (CKD) and why is it a concern?
-Anemia in CKD refers to a condition where the patient has a lower than normal number of red blood cells (hemoglobin levels). It is a concern because it can worsen the patient's quality of life, increase the risk of cardiovascular diseases, and accelerate kidney function decline. The condition is caused by a variety of factors, including reduced erythropoietin production and iron deficiency.
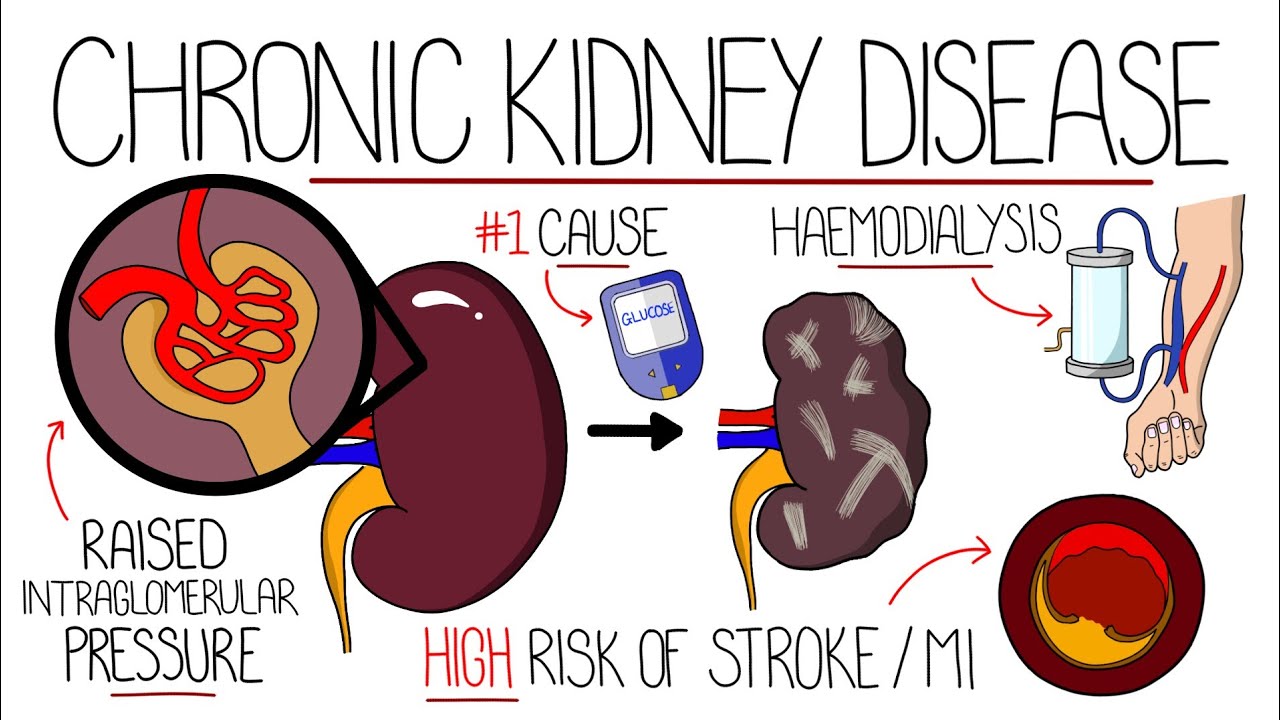
How does CKD contribute to the development of anemia?
-CKD contributes to anemia in several ways. The kidney’s reduced function leads to decreased production of erythropoietin, a hormone crucial for red blood cell production. Additionally, CKD patients often experience iron deficiency, shortened red blood cell lifespan, and chronic inflammation, all of which exacerbate anemia.
What is the relationship between erythropoietin and red blood cell formation?
-Erythropoietin is a hormone produced primarily by the kidneys. It stimulates the bone marrow to produce red blood cells. In CKD, the kidneys' ability to produce erythropoietin is impaired, leading to reduced red blood cell production and anemia.
Why do iron and hepcidin play critical roles in anemia in CKD?
-Iron is essential for the production of hemoglobin in red blood cells. Hepcidin, a protein produced by the liver, regulates iron levels in the body. In CKD, inflammation increases hepcidin levels, which reduces iron absorption in the gut and hampers iron availability for red blood cell production, worsening anemia.
What are the common symptoms of anemia in CKD?
-Common symptoms of anemia in CKD include fatigue, weakness, shortness of breath, dizziness, headaches, and palpitations. Patients may also experience exercise intolerance and chest pain due to reduced oxygen delivery to tissues, including the heart.
How does anemia in CKD affect the heart?
-Anemia in CKD leads to insufficient oxygen delivery to the heart and other organs. As a result, the heart compensates by pumping more blood, which can eventually lead to heart strain, hypertrophy (thickening of the heart muscle), and potentially heart failure if left untreated.
What is the target hemoglobin level for CKD patients with anemia?
-The target hemoglobin (Hb) level for CKD patients with anemia is typically between 11 and 12 g/dL. Maintaining Hb levels above 13 g/dL is not recommended, as it could increase risks without additional benefits.
What are the primary treatments for anemia in CKD?
-The primary treatments for anemia in CKD include erythropoiesis-stimulating agents (ESA), iron supplementation, and correction of underlying causes such as chronic inflammation or vitamin deficiencies. Dialysis optimization and management of secondary hyperparathyroidism are also crucial in managing anemia.
When should erythropoiesis-stimulating agents (ESA) be used in CKD?
-ESAs should be used in CKD patients whose hemoglobin levels are below 10 g/dL, but only after ensuring adequate iron levels. ESA therapy helps stimulate red blood cell production, improving anemia and its associated symptoms.
What factors should be considered before administering ESA in CKD patients?
-Before administering ESA, it is essential to evaluate the patient’s iron status, ensuring that ferritin levels are above 200 ng/mL and transferrin saturation is above 20%. ESA should not be given unless there is sufficient iron available to support red blood cell production.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade Now5.0 / 5 (0 votes)