Chronic kidney disease - causes, symptoms, diagnosis, treatment, pathology
Summary
TLDRThis script explains chronic kidney disease (CKD), a condition where kidney function declines over three months or more, contrasting it with acute kidney injury. It details the kidney's role in blood regulation, the impact of hypertension and diabetes on kidney health, and the process leading to glomerulosclerosis and CKD. It also covers complications like electrolyte imbalances, toxin accumulation, hypertension, and bone disorders. Diagnosis involves monitoring the glomerular filtration rate (GFR), with treatments ranging from managing underlying causes to dialysis or kidney transplant.
Takeaways
- 🩺 Chronic kidney disease (CKD) involves a gradual decline in kidney function over at least three months, while acute kidney injury occurs within less than three months.
- 🩸 The kidneys regulate blood by removing waste, balancing electrolytes, managing water levels, and producing hormones.
- 💉 Glomerular filtration rate (GFR) measures how much fluid is filtered by the kidneys per minute; a normal rate is around 100-120 ml/min/1.73 m².
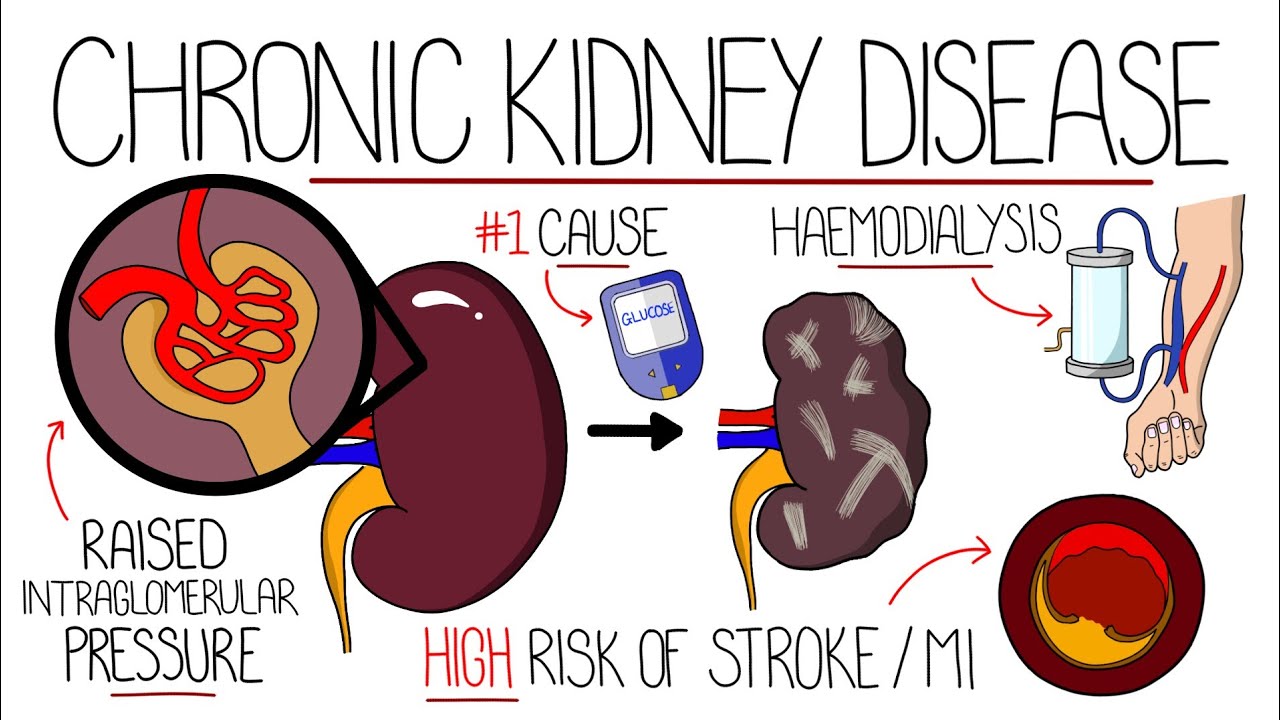
- 🔍 Hypertension is a common cause of CKD, leading to thickened artery walls and reduced blood supply, causing ischemic injury and glomerulosclerosis.
- 🍬 Diabetes is the leading cause of CKD, where excess glucose causes stiffening of the efferent arteriole, leading to hyperfiltration and glomerulosclerosis.
- ⚠️ Other causes of CKD include systemic diseases like lupus, infections like HIV, long-term use of NSAIDs, and exposure to toxins like tobacco.
- 🧠 Accumulation of toxins due to decreased GFR can cause azotemia, encephalopathy, pericarditis, and uremic frost, affecting the central nervous system and other body functions.
- ⚡ CKD can lead to hyperkalemia due to reduced potassium excretion, causing potentially dangerous cardiac arrhythmias.
- 🦴 CKD disrupts calcium and vitamin D balance, leading to hypocalcemia and renal osteodystrophy, weakening bones.
- 🔄 CKD creates a vicious cycle where decreased kidney function triggers renin secretion, leading to hypertension, which further damages the kidneys.
Q & A
What is the difference between chronic kidney disease and acute kidney injury in terms of the time frame of kidney function decline?
-Chronic kidney disease involves a gradual decrease in kidney function that develops over a minimum of three months, whereas acute kidney injury refers to a rapid deterioration in kidney function that occurs in less than three months.
What are the primary functions of the kidneys?
-The kidneys' primary functions include regulating blood composition by removing waste, maintaining steady electrolyte levels, regulating the overall amount of water, and producing hormones.
How does blood enter the kidney and where does the initial filtration occur?
-Blood enters the kidney through the renal artery and is initially filtered in tiny clumps of arterioles called glomeruli.
What is the glomerular filtration rate (GFR) and what is the normal range for a healthy person?
-The glomerular filtration rate (GFR) is the rate at which blood is filtered in the kidneys. In a normal, healthy person, it is approximately 100-120 milliliters of fluid filtered per minute per 1.73 m2 of body surface area.
How does hypertension contribute to the development of chronic kidney disease?
-Hypertension causes the walls of arteries supplying the kidney to thicken, resulting in a narrowed lumen and less blood and oxygen delivery to the kidney. This leads to ischemic injury and the subsequent development of glomerulosclerosis, which diminishes the nephron's ability to filter blood.
What is the role of Transforming Growth Factor ß1 (TGF-ß1) in the progression of chronic kidney disease?
-TGF-ß1 is a growth factor secreted by immune cells in response to kidney damage. It causes mesangial cells to revert to a less mature state and secrete extracellular matrix, leading to glomerulosclerosis and reduced nephron function over time.
How does diabetes lead to chronic kidney disease?
-In diabetes, excess glucose in the blood undergoes non-enzymatic glycation, particularly affecting the efferent arteriole and causing it to become stiff and narrow, a process known as hyaline arteriosclerosis. This leads to hyperfiltration and eventual glomerulosclerosis, impairing the nephron's ability to filter blood.
What are some other causes of chronic kidney disease besides diabetes and hypertension?
-Other causes of chronic kidney disease include systemic diseases like lupus and rheumatoid arthritis, infections such as HIV, and long-term use of medications like NSAIDs, as well as exposure to toxins found in tobacco.
What is azotemia and what symptoms can it cause?
-Azotemia is a condition where urea accumulates in the blood due to decreased glomerular filtration rate. It can cause general symptoms such as nausea and loss of appetite.
How does chronic kidney disease affect the balance of electrolytes like potassium and calcium?
-In chronic kidney disease, less potassium is excreted, leading to hyperkalemia, which can cause cardiac arrhythmias. Additionally, less activated vitamin D results in hypocalcemia, causing calcium to be resorbed from bones, leading to renal osteodystrophy.
What is the role of the hormone renin in chronic kidney disease and its relationship with hypertension?
-Renin is released by the kidneys in response to a lower than normal amount of fluid being filtered. In chronic kidney disease, the falling GFR leads to increased renin secretion, which in turn raises blood pressure, contributing to hypertension and creating a vicious cycle.
How is anemia related to chronic kidney disease and what hormone is involved in this process?
-Anemia in chronic kidney disease is related to the reduced secretion of the hormone erythropoietin, which stimulates red blood cell production. Lower levels of erythropoietin lead to decreased red blood cell production.
What diagnostic methods are used to confirm chronic kidney disease?
-The diagnosis of chronic kidney disease is based on monitoring changes in the glomerular filtration rate over time. A GFR of less than 90 ml/min/1.73 m2 may suggest the disease, and irreversible kidney damage may occur with a GFR below 60 ml/min/1.73 m2. A kidney biopsy can confirm the diagnosis by identifying changes like glomerulosclerosis.
What are the general treatment approaches for chronic kidney disease?
-Treatment for chronic kidney disease often involves managing the underlying cause. In severe cases, dialysis or a kidney transplant may be necessary.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Kidney injuries 2
Postrenal acute kidney injury (acute renal failure) - causes, symptoms, & pathology
Understanding Chronic Kidney Disease (CKD)

Kidney Scientist Reveals How High Protein Affects the Human Body (kidneys & other organs)
Chronic Renal Failure (Chronic Kidney Disease) ESRD l Nursing NCLEX RN & LPN

Chronic kidney disease: Clinical Nursing Care
5.0 / 5 (0 votes)