Understanding Chronic Kidney Disease (CKD)
Summary
TLDRChronic Kidney Disease (CKD) is a progressive and irreversible condition affecting kidney function. It is categorized into five stages based on glomerular filtration rate (GFR), with stage 5 being end-stage renal disease. Causes include type 2 diabetes, hypertension, and kidney damage from various intrinsic and extrinsic factors. Early CKD is often asymptomatic, but as it progresses, complications like cardiovascular risks, anemia, metabolic acidosis, and bone issues arise. Treatment focuses on managing risk factors and complications, with options ranging from medication and lifestyle changes to renal replacement therapies like dialysis and kidney transplantation.
Takeaways
- 😀 Chronic kidney disease (CKD) is a progressive and irreversible condition characterized by reduced kidney function or damage for over three months.
- 😀 The glomerular filtration rate (GFR) is used to classify CKD into stages, with GFR below 15 indicating end-stage renal disease, often requiring dialysis or a transplant.
- 😀 CKD can be asymptomatic initially, but as it progresses, it can lead to severe complications such as cardiovascular risks, stroke, anemia, metabolic acidosis, and bone issues.
- 😀 The most common causes of CKD are type 2 diabetes (30-50% of cases) and hypertension, with other causes including kidney damage from diabetes and intrinsic conditions.
- 😀 CKD can result in fluid overload, leading to pulmonary edema, peripheral edema, and ascites, due to the kidney's reduced ability to excrete sodium.
- 😀 Anemia in CKD is due to reduced erythropoietin production and chronic disease-related inflammation, leading to symptoms like fatigue and shortness of breath.
- 😀 CKD leads to metabolic acidosis, further exacerbating anemia and causing issues like hypokalemia and hyperkalemia, which contribute to further kidney damage.
- 😀 The kidney regulates calcium and phosphate balance, and CKD causes lower calcium levels, leading to higher parathyroid hormone levels and affecting bone remodeling.
- 😀 Common diagnostic tests for CKD include GFR, albumin-to-creatinine ratio in urine, and imaging such as ultrasound or CT scans to identify structural changes and complications.
- 😀 Treatment for CKD focuses on controlling risk factors like hyperglycemia and hypertension, lifestyle changes, medications like ACE inhibitors, SGLT2 inhibitors, and potentially renal replacement therapies such as dialysis or transplant.
Q & A
What is chronic kidney disease (CKD)?
-Chronic kidney disease (CKD) is a progressive, irreversible condition characterized by a decrease in kidney function or kidney damage lasting more than three months.
How is CKD classified into stages?
-CKD is classified into five stages based on the Glomerular Filtration Rate (GFR), which measures how well the kidneys are filtering waste. Stages range from Stage 1 (mild) to Stage 5 (end-stage renal disease).
What does a GFR value below 60 indicate?
-A GFR below 60 milliliters per minute indicates a reduced kidney function, which can be classified as CKD. A GFR below 15 is classified as end-stage renal disease, requiring dialysis or a kidney transplant.
What are the common causes of CKD?
-The most common causes of CKD are Type 2 diabetes (30-50%), hypertension, and genetic conditions like polycystic kidney disease. Other factors include pre-renal conditions like chronic heart failure or cirrhosis.
How can CKD affect cardiovascular health?
-CKD significantly raises cardiovascular risk, with patients being 5-10 times more likely to die from cardiovascular disease. The risk of stroke increases as the GFR declines, and CKD can contribute to hypertension and fluid overload, both of which strain the heart.
What complications are associated with CKD?
-Complications of CKD include cardiovascular disease, anemia (due to reduced erythropoietin production), metabolic acidosis, bone damage, fluid overload, and high urea levels, which can lead to lethargy or even encephalopathy.
What is the role of the kidney in calcium and phosphate regulation?
-The kidneys regulate calcium and phosphate by activating vitamin D via the enzyme 1-alpha-hydroxylase. CKD impairs this process, leading to low calcium levels, which in turn raises parathyroid hormone and affects bone health.
How is CKD diagnosed?
-CKD is diagnosed through tests that measure kidney function, such as GFR and the albumin-to-creatinine ratio. Additional tests include urinalysis to detect proteinuria or hematuria, and imaging studies like ultrasound to identify structural abnormalities.
What are the treatment strategies for CKD?
-Treatment for CKD focuses on slowing progression and managing complications. This includes controlling risk factors like blood sugar and blood pressure, medications (ACE inhibitors, SGLT2 inhibitors), lifestyle changes (low-salt, low-protein diet), and possibly renal replacement therapy in later stages.
What is the role of renal replacement therapy in CKD?
-Renal replacement therapy, including dialysis or kidney transplant, is used when kidney function deteriorates significantly (stage 5). Dialysis can be hemodialysis (via a machine) or peritoneal dialysis (using the peritoneal cavity), and a kidney transplant is a permanent solution.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Chronic kidney disease: Clinical Nursing Care

Kidney injuries 2
Chronic kidney disease - causes, symptoms, diagnosis, treatment, pathology
Chronic Renal Failure (Chronic Kidney Disease) ESRD l Nursing NCLEX RN & LPN
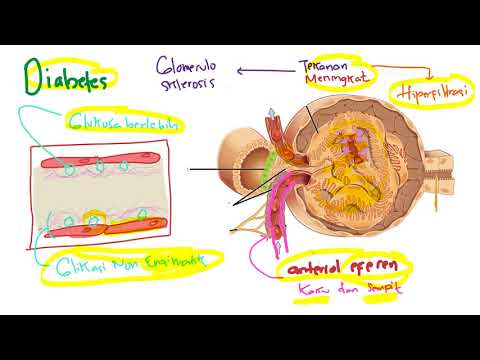
Patofisiologi - Penyakit Ginjal Kronis (PGK) / Chronic kidney disease (CKD)

Kidney Scientist Reveals How High Protein Affects the Human Body (kidneys & other organs)
5.0 / 5 (0 votes)