Asthma - signs and symptoms, pathophysiology
Summary
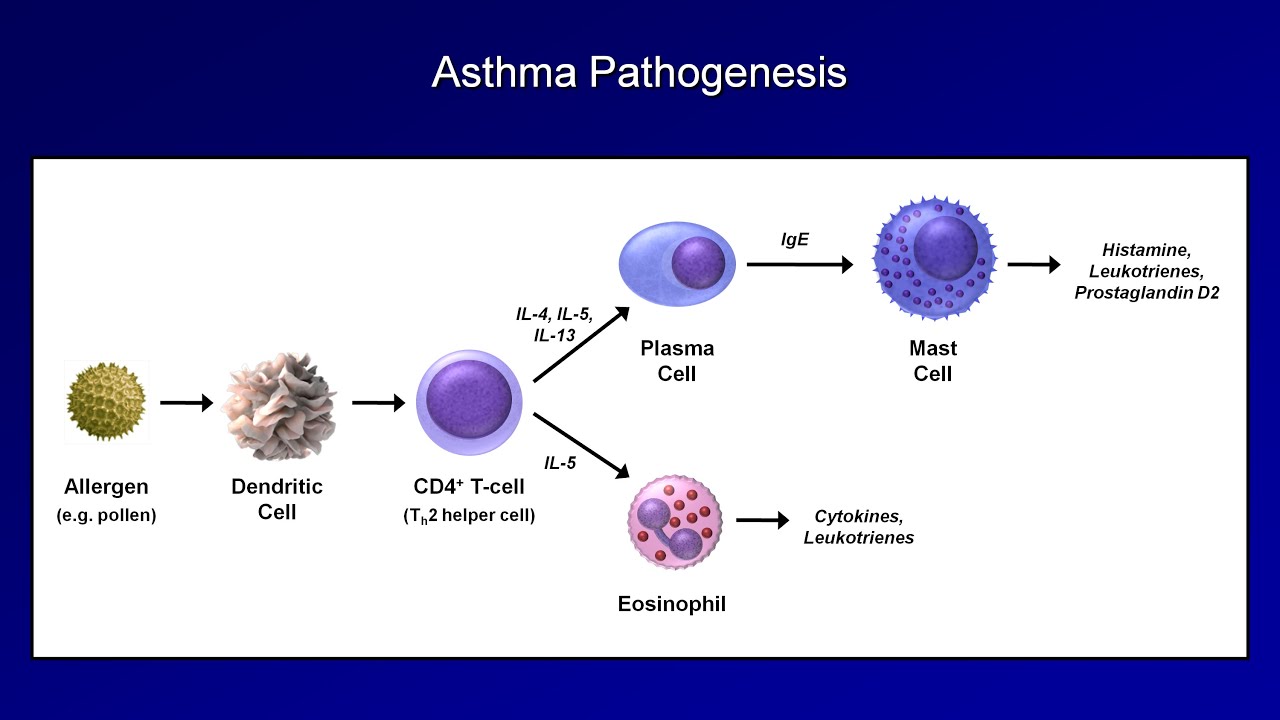
TLDRIn this educational video, Armando delves into asthma, a chronic inflammatory airway disorder, distinguishing between atopic (environmentally triggered) and non-atopic (intrinsic) types. He illustrates the structural differences in bronchial layers between normal and asthmatic lungs, highlighting increased mucus production, thickened basement membranes, and heightened immune cell activity. The video explores the pathophysiology, focusing on the role of IgE antibodies, mast cells, and T-helper cells, particularly the imbalance between T-helper 1 and T-helper 2 cells in asthma. It concludes with the pathogenesis of atopic asthma, detailing how allergens trigger a cascade of responses leading to bronchoconstriction and inflammation.
Takeaways
- 🌟 Asthma is a chronic inflammatory disorder of the airways, which can be categorized into atopic (extrinsic, triggered by environmental factors) and non-atopic (intrinsic, not allergen-induced).
- 🔬 In atopic asthma, systemic IgE production mediates inflammation, while non-atopic asthma involves local IgE production without allergen exposure.
- 👤 The cross-section of a normal lung includes a mucous layer, pseudostratified columnar epithelial cells, lamina propria, and smooth muscles, which are altered in asthmatic bronchioles.
- 🌬️ Asthma is characterized by airflow obstruction, bronchial hyperresponsiveness due to histamine release, and inflammation from increased neutrophils and immune cells.
- 🤧 Symptoms of asthma include shortness of breath, wheezing, chest tightness, and a dry, irritating cough.
- 🧬 IgE antibodies play a crucial role in asthma by binding to mast cells, leading to the release of histamine and other inflammatory mediators upon allergen exposure.
- 🔄 T-helper cells, particularly T-helper 2 cells, are up-regulated in asthma and promote inflammation through humoral immunity and increased antibody production.
- 🚨 The pathophysiology of asthma involves a complex interplay of cells like mast cells, dendritic cells, and T-helper cells, which contribute to the inflammatory response.
- 🛡️ The body's response to allergens in asthma includes the activation of dendritic cells, T-helper cells, and the production of IgE antibodies, leading to a cascade of events that result in airway constriction and inflammation.
- 🔙 The presence of IgE antibodies creates a memory response, so that subsequent exposures to the same allergen can trigger a rapid and severe asthmatic reaction.
Q & A
What is asthma defined as?
-Asthma is defined as a chronic inflammation disorder of the airways.
How can asthma be categorized?
-Asthma can be divided into atopic and non-atopic. Atopic asthma is extrinsic, triggered by environmental factors, and is the most common. Non-atopic asthma is intrinsic and less common, involving inflammation and constriction not caused by allergen exposure.
What are the main features of a normal bronchial layer?
-A normal bronchial layer features a mucus layer, pseudostratified columnar epithelial cells, a basement membrane, lamina propria containing various cells including macrophages and mast cells, and two smooth muscles.
What changes occur in the bronchial layer in asthmatics?
-In asthmatics, there is an increase in mucus production and goblet cells, thickening of the basement membrane, an increase in mast cell numbers in the lamina propria, and smooth muscle cell hypertrophy due to constriction.
What are the three characteristics of asthma known as?
-The three characteristics of asthma are airflow obstruction, bronchial hyperresponsiveness due to histamine release, and inflammation due to an increase in neutrophils and other immune cells.
What are the common symptoms of asthma?
-Symptoms of asthma include shortness of breath, wheezing, chest tightness, and a dry, irritating cough.
What is the role of IgE antibodies in the pathophysiology of asthma?
-IgE antibodies bind to receptors on mast cells, forming a mast cell IgE complex that recognizes allergens and triggers the release of histamine and other inflammatory mediators.
How do T helper cells contribute to asthma?
-In asthma, T helper 2 cells are up-regulated and promote inflammation by increasing humoral immunity, stimulating IgE production, and promoting mast cell activity and eosinophil production.
What is the process that occurs when an asthmatic inhales an allergen?
-When an asthmatic inhales an allergen, it is engulfed by dendritic cells and activates them. This leads to the production of chemokines that attract T helper 2 cells, which in turn stimulate the production of IgE and promote inflammation, leading to bronchoconstriction and other asthma symptoms.
How does the presence of IgE lead to bronchoconstriction?
-The inhaled allergen binds to the IgE-mast cell complex, causing the mast cell to release histamine, prostaglandins, and leukotrienes, which stimulate the smooth muscles in the airways to constrict, leading to bronchoconstriction.
What is the significance of the increase in eosinophils in asthma?
-The increase in eosinophils in asthma is significant because they are involved in the inflammatory response, contributing to the constriction and inflammation of the airways, which are characteristic features of asthma.
Outlines

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードMindmap

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードKeywords

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードHighlights

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードTranscripts

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレード関連動画をさらに表示
Eczema (Atopic Dermatitis) | Atopic Triad, Triggers, Who gets it, Why does it happen, & Treatment

Curso de Farmacologia: Aula 38 - Farmacologia da asma e DPOC (1a parte)

Pharmacology - DRUGS FOR ASTHMA AND COPD (MADE EASY)

Pharmacology: Drugs for Asthma and COPD, Animation
Asthma and COPD - Pathogenesis and Pathophysiology

INFLAMASI PADA AUTOIMUN - dr. Sarah Akbari, MARS, ABAARM, FAARM, FINEM
5.0 / 5 (0 votes)
