Pharmacology - DRUGS FOR ASTHMA AND COPD (MADE EASY)
Summary
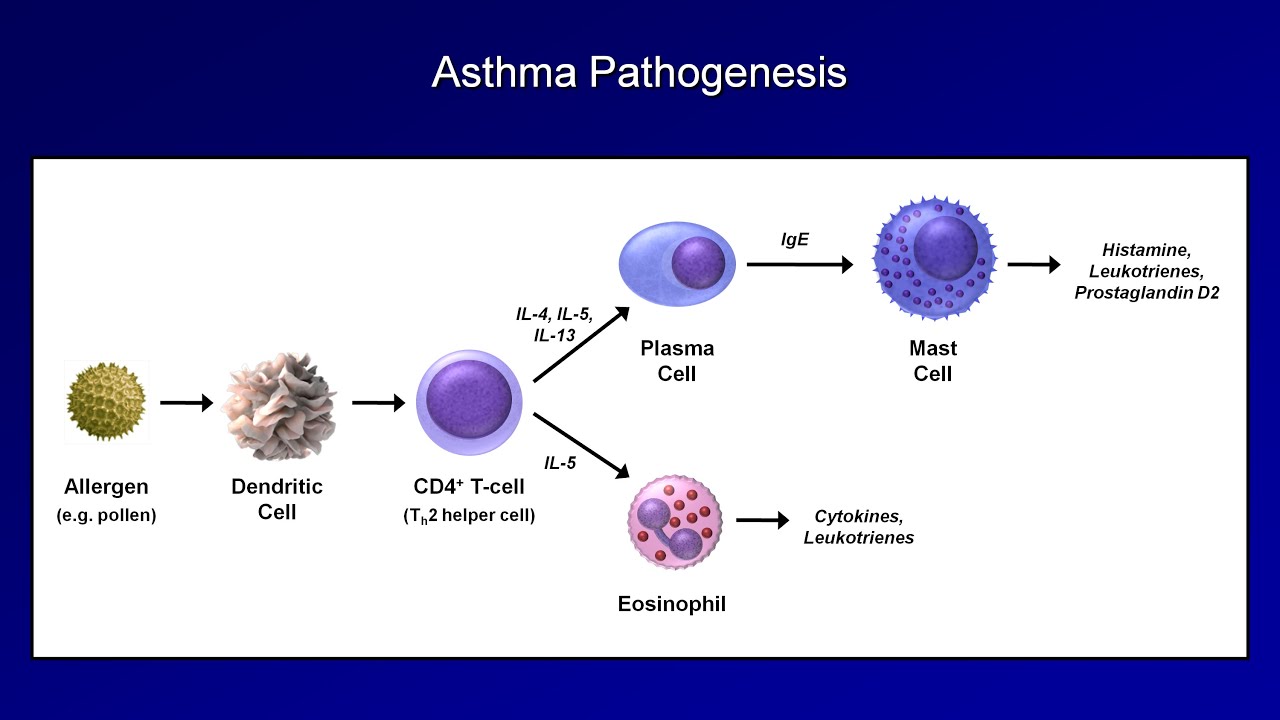
TLDRThis lecture delves into the pharmacology of asthma and COPD treatments, highlighting the distinct pathophysiologies of both diseases. It explains the roles of mast cells in asthma and macrophages in COPD, detailing the inflammatory processes and bronchoconstriction. The video outlines various drug classes used in treatment, such as inhaled beta-2 agonists, muscarinic antagonists, leukotriene modifiers, and corticosteroids, emphasizing their mechanisms of action in managing airway inflammation and constriction.
Takeaways
- 🌟 Asthma and COPD are chronic lung diseases characterized by inflammation and narrowing of the airways, but they have distinct pathophysiologies.
- 🔬 Mast cells are key in asthma, activated by inhaled allergens to release bronchoconstrictor mediators, while macrophages orchestrate inflammation in COPD, often due to cigarette smoke.
- 💊 Inhaled beta-2 adrenergic agonists are used in both asthma and COPD to improve airflow by increasing cAMP levels and relaxing smooth muscles.
- 🍃 Muscarinic antagonists, or anticholinergics, block the effects of acetylcholine, reducing bronchial smooth muscle contraction in asthma and COPD.
- 🧬 Leukotriene modifiers target the action of leukotrienes, which are potent bronchoconstrictors produced by mast cells in asthma.
- ⚗️ Phosphodiesterase inhibitors like Theophylline and Roflumilast affect bronchodilation by influencing the breakdown of cAMP in smooth muscle cells.
- 💉 Omalizumab is a monoclonal antibody for allergic asthma that binds to free IgE, preventing mast cell degranulation and release of bronchoconstrictor mediators.
- 💦 Antihistamines reduce histamine-mediated responses by inhibiting the function of H1 receptors in allergic asthma.
- 🌿 Corticosteroids are used to suppress airway inflammation by affecting gene expression at the genetic level, both in asthma and COPD.
- 🛡️ Corticosteroids' anti-inflammatory effects involve binding to coactivators and histone deacetylase to suppress inflammatory genes or activate anti-inflammatory genes.
- 💥 Theophylline and Roflumilast differ in their mechanism of PDE inhibition, with Roflumilast being more selective and potentially safer.
Q & A
What are the main characteristics of asthma and COPD?
-Asthma and COPD are chronic lung diseases characterized by inflammation and narrowing of the airways. They share some features but have distinct pathophysiologies.
What role do mast cells play in the pathophysiology of asthma?
-Mast cells are key in asthma pathophysiology, being abundant in the airways of asthmatic patients and releasing bronchoconstrictor mediators upon activation by inhaled allergens.
How do inhaled allergens activate mast cells in asthma?
-Inhaled allergens activate sensitized mast cells by crosslinking surface-bound IgE molecules, leading to the release of various bronchoconstrictor mediators.
What is the significance of thymic stromal lymphopoietin (TSLP) in the pathophysiology of asthma?
-TSLP is secreted by epithelial and mast cells and conditions dendritic cells to release chemokines that attract T helper 2 cells, contributing to the allergic response in asthma.
What are the main mediators released by activated mast cells that contribute to bronchoconstriction and inflammation?
-Activated mast cells release granule-derived mediators like histamine and newly formed metabolites of arachidonic acid, such as prostaglandins and leukotrienes, which promote inflammation and induce bronchoconstriction.
Why are cysteinyl leukotrienes considered potent bronchoconstrictors?
-Cysteinyl leukotrienes (LTC4, LTD4, and LTE4) are potent bronchoconstrictors because they activate Gq protein-coupled CysLT1 receptors on bronchial smooth muscle cells, increasing intracellular calcium concentration and causing smooth muscle contraction.
How do adenosine and histamine contribute to bronchoconstriction?
-Adenosine activates Gi protein-coupled adenosine A1 receptors on bronchial smooth muscle cells, decreasing cyclic AMP levels and leading to smooth muscle contraction. Histamine causes smooth muscle contraction by activating Gq protein-coupled H1 receptors.
What is the role of inhaled beta-2 adrenergic agonists in treating asthma and COPD?
-Inhaled beta-2 adrenergic agonists improve airflow by increasing cAMP levels upon receptor activation, leading to smooth muscle relaxation and bronchodilation.
What are the two types of beta-2 adrenergic agonists and their duration of action?
-There are short-acting beta-2 agonists (SABAs) that provide bronchodilation for about 4 to 6 hours, and long-acting beta-2 agonists (LABAs) that provide bronchodilation for about 12 hours.
How do muscarinic antagonists, or anticholinergics, work in the treatment of asthma and COPD?
-Muscarinic antagonists block the effects of acetylcholine on muscarinic receptors involved in bronchial smooth muscle contraction, leading to reduced intracellular calcium concentrations and airway smooth muscle relaxation.
What is the primary effect of corticosteroids in suppressing airway inflammation?
-Corticosteroids primarily affect the genetic level by suppressing activated inflammatory genes and activating anti-inflammatory genes, which helps to reduce airway inflammation.
How do corticosteroids influence the inflammatory gene activation process?
-Corticosteroids, depending on the dose, can bind to cytoplasmic glucocorticoid receptors and translocate to the nucleus, where they inhibit histone acetyltransferase activity, recruit histone deacetylase, or bind to glucocorticoid response elements to activate anti-inflammatory genes.
What is the mechanism of action of Theophylline and Roflumilast in treating airway constriction?
-Theophylline binds to adenosine A1 receptors to block adenosine-mediated bronchoconstriction and nonselectively inhibits phosphodiesterases, contributing to bronchodilation. Roflumilast selectively inhibits phosphodiesterase-4 (PDE-4), improving therapeutic efficacy and safety profile compared to Theophylline.
What are the two pharmacotherapeutic options specifically for patients with allergic asthma mentioned in the script?
-Omalizumab, a monoclonal antibody that binds to free IgE and prevents mast cell degranulation, and antihistamines, which inhibit the function of H1 receptors to reduce histamine-mediated responses.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Curso de Farmacologia: Aula 38 - Farmacologia da asma e DPOC (1a parte)

Pharmacology: Drugs for Asthma and COPD, Animation
Asthma and COPD - Pathogenesis and Pathophysiology

Interview with Dr. Andra Fee, Pulmonologist at Meadville Medical Center

Pharmacology - GASTROINTESTINAL AND ANTIEMETIC DRUGS (MADE EASY)
Introduction to Pathology - Cell Injury - A New Pathology Series
5.0 / 5 (0 votes)