Asthma and COPD - Pathogenesis and Pathophysiology
Summary
TLDRThis video explores the pathogenesis and pathophysiology of asthma and COPD, emphasizing the immune system's role in both conditions. It discusses the activation of Th2 cells and the subsequent inflammatory response in asthma, highlighting the role of eosinophils and mast cells. In contrast, COPD primarily results from cigarette smoke-induced inflammation, leading to airway obstruction and structural lung changes. The video also outlines key differences in clinical manifestations between asthma and COPD, providing a comprehensive understanding of these obstructive lung diseases.
Takeaways
- 😀 Asthma and COPD are both types of obstructive lung diseases with distinct pathophysiological mechanisms.
- 💡 The immune system plays a critical role in the pathogenesis of asthma, particularly through the activation of T helper 2 cells.
- 🔬 In asthma, exposure to allergens triggers dendritic cells to present these antigens to T lymphocytes, leading to a chain of immune responses.
- 📊 Key mediators in asthma include IL-4, IL-5, and IL-13, which promote eosinophil activation and IgE production.
- 🚨 Acute responses in asthma result in bronchospasm, airway edema, and increased mucus production, leading to airway obstruction.
- 📈 Chronic exposure to allergens can lead to airway hyperresponsiveness and structural changes in the airway, even during symptom-free periods.
- 🚬 COPD is predominantly caused by cigarette smoke, which triggers chronic inflammation via alveolar macrophages and CD8 T cells.
- ⚠️ The pathophysiological processes in COPD include airway obstruction, hyperinflation, and impaired gas exchange due to lung parenchyma destruction.
- 🌡️ Symptoms of COPD can include chronic cough, mucus plugs, and signs of right heart failure (cor pulmonale).
- 🔄 Understanding the differences in inflammation between asthma (primarily proximal airways) and COPD (distal airways and lung parenchyma) is essential for effective diagnosis and management.
Q & A
What are the primary learning objectives of the video on obstructive lung disease?
-The primary learning objectives are to describe the immune system's role in the pathogenesis of asthma and COPD, comparing the mechanisms of inflammation in each, and to explain the pathophysiology of COPD, including hypercapnia and hypoxemia.
How does the immune system contribute to the pathogenesis of asthma?
-In asthma, exposure to an inhaled allergen triggers dendritic cells to present the allergen to T helper type 2 (Th2) cells, leading to the release of interleukins that activate eosinophils and plasma cells, resulting in an inflammatory response.
What are the main chemical mediators involved in asthma?
-The key chemical mediators in asthma include interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-13 (IL-13), which are involved in the activation of immune cells and the inflammatory process.
What distinguishes allergic asthma from intrinsic asthma?
-Allergic (extrinsic) asthma typically presents in children and is triggered by environmental allergens, while intrinsic asthma occurs in adults and is often triggered by irritants like cigarette smoke or air pollution, without a clear allergic component.
What role does cigarette smoke play in the development of COPD?
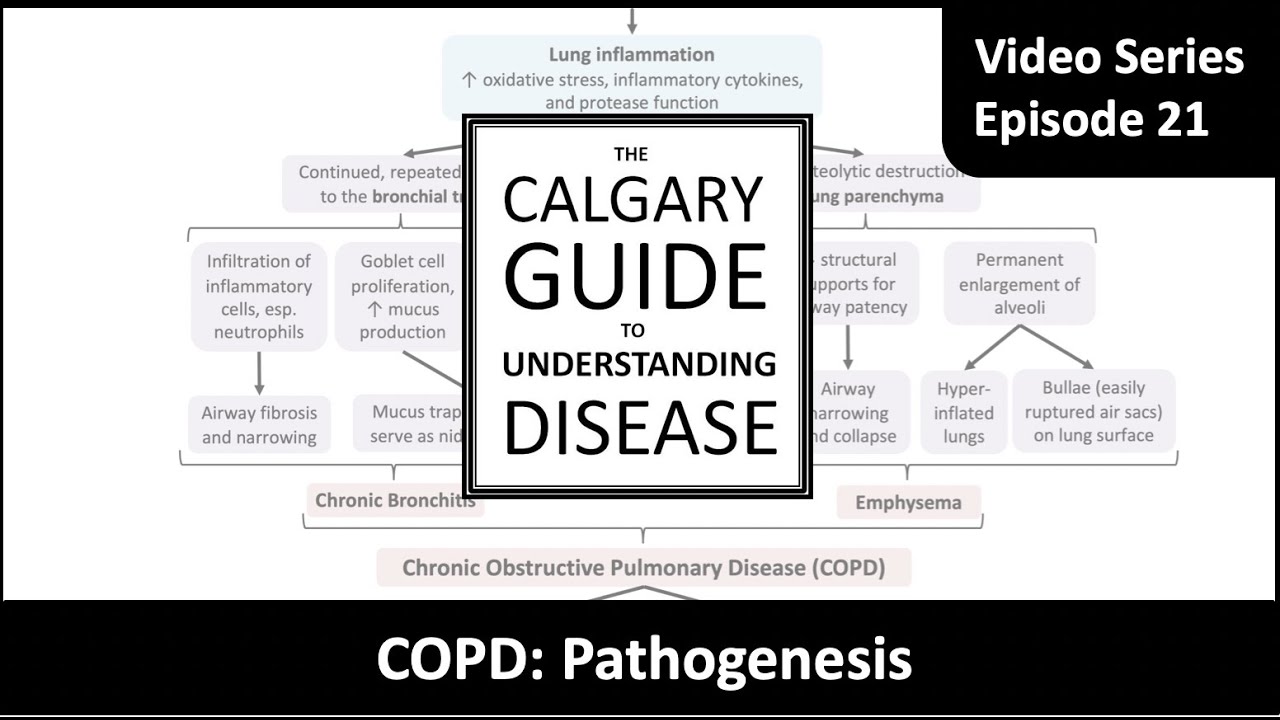
-Cigarette smoke is the primary cause of COPD, activating alveolar macrophages and leading to chronic inflammation, which results in airway remodeling, increased mucus production, and destruction of lung parenchyma.
What are the physiological consequences of chronic inflammation in COPD?
-Chronic inflammation in COPD leads to airway fibrosis, mucus hyperplasia, and destruction of lung parenchyma, resulting in airway obstruction, hyperinflation, and impaired gas exchange.
How is hypercapnia related to COPD?
-Hypercapnia in COPD results from airway obstruction and hypoventilation, leading to decreased tidal volume and impaired gas exchange, causing elevated carbon dioxide levels in the blood.
What mechanisms contribute to hypoxemia in patients with COPD?
-Hypoxemia in COPD can be caused by hypoventilation leading to low arterial oxygen levels, ventilation-perfusion mismatching due to uneven airflow and blood flow, and decreased diffusion capacity from lung destruction.
How are patients with COPD classified into 'blue bloaters' and 'pink puffers'?
-'Blue bloaters' are typically patients with chronic bronchitis characterized by significant hypoxemia and right heart failure, while 'pink puffers' have emphysema, where hypoxemia is less severe, but they often experience increased work of breathing and weight loss.
What is the significance of understanding the differences in inflammation between asthma and COPD?
-Understanding the differences in inflammation helps clinicians tailor treatment approaches, as asthma primarily involves Th2 cells and eosinophils, while COPD involves CD8 T cells and neutrophils, affecting management strategies for each condition.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Asthma - signs and symptoms, pathophysiology

Curso de Farmacologia: Aula 38 - Farmacologia da asma e DPOC (1a parte)

Pharmacology - DRUGS FOR ASTHMA AND COPD (MADE EASY)

Common Diseases of Respiratory System, What are the common diseases of lungs? Respiratory disorders
COPD Pathogenesis

Hypersensitivity Part II|Simplified Explanation|Immunology|Allergy|Immune System|IgG & IgM Antibody|
5.0 / 5 (0 votes)