Pharmacology - ANTIARRHYTHMIC DRUGS (MADE EASY)
Summary
TLDRThis lecture delves into the world of antiarrhythmic drugs, explaining the heart's electrical system and how it controls the heartbeat. It covers the role of specialized cells, the conduction system, and the action potential differences between pacemaker and cardiac muscle cells. The script also explores arrhythmias, their mechanisms, and the Vaughan Williams classification of antiarrhythmic drugs, detailing the function and effects of each class. Additionally, it touches on other agents like Digoxin, Adenosine, and Magnesium Sulfate, concluding with their applications in treating various cardiac conditions.
Takeaways
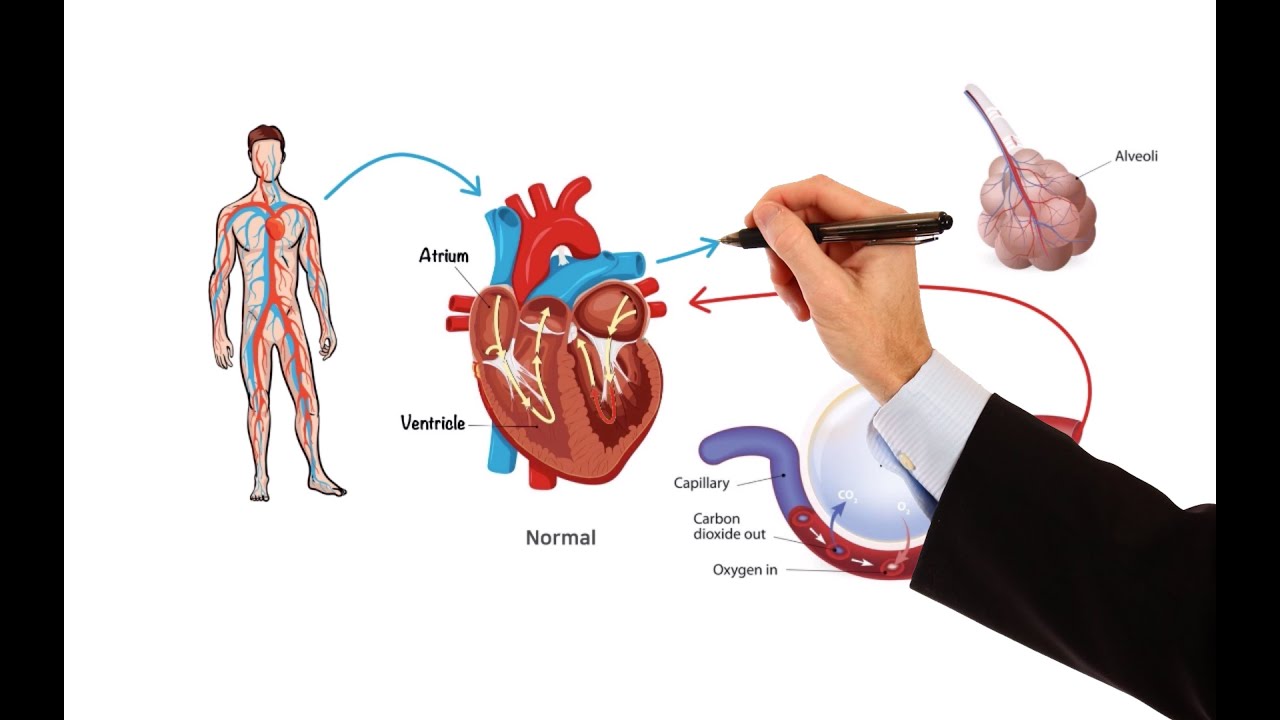
- 💓 The heart's pumping action is controlled by its electrical system, involving specialized cells that generate and transmit electrical impulses to the cardiac muscle.
- 🔌 The cardiac conduction system consists of five elements: the sinoatrial (SA) node, atrioventricular (AV) node, bundle of His, bundle branches, and Purkinje fibers, which coordinate the heart's rhythm.
- 📈 The normal heart rhythm is initiated by the SA node and is represented on an electrocardiogram (ECG) by the P wave for atrial contraction, the PR interval for AV node delay, the QRS complex for ventricular contraction, and the T wave for ventricular recovery.
- 🔑 Cardiac cells are divided into contractile cells that generate force for heart contraction and conducting cells that initiate electrical impulses, with the latter exhibiting automaticity.
- 🌡️ The action potential of pacemaker cells differs from that of cardiac muscle cells, with pacemaker cells having a resting membrane potential of about -60 mV and undergoing a unique depolarization process.
- 🚫 Arrhythmias are deviations from the normal heart rhythm, classified as bradyarrhythmias (<60 bpm) or tachyarrhythmias (>100 bpm), with the latter involving mechanisms like abnormal automaticity, triggered activity, and reentry.
- 🛡️ Vaughan Williams classification categorizes antiarrhythmic drugs into four classes based on their primary mechanism of action, influencing sodium and calcium channels, and potassium channels, among others.
- 💊 Class 1 antiarrhythmics, such as Procainamide, Quinidine, and Disopyramide, work by blocking sodium channels to slow down depolarization and are used for various arrhythmias but can cause adverse effects.
- 🛡️ Class 2 drugs are beta blockers that reduce heart rate and contractility, useful for arrhythmias caused by increased sympathetic activity, with examples like Propranolol and Metoprolol.
- 🔋 Class 3 agents, including Amiodarone and Dronedarone, block potassium channels to prolong the action potential and are effective against atrial fibrillation and ventricular tachyarrhythmias but can have significant side effects.
- 🚰 Class 4 drugs, like Verapamil and Diltiazem, block calcium channels to slow conduction in the SA and AV nodes, treating supraventricular tachycardia and atrial fibrillation.
- 🌿 Other antiarrhythmic agents not fitting into the Vaughan Williams classes include Digoxin, which enhances contractility and slows AV node conduction, Adenosine for acute supraventricular tachycardia, and Magnesium Sulfate for specific arrhythmias like torsades de pointes.
Q & A
What are antiarrhythmic drugs and why are they important?
-Antiarrhythmic drugs are medications used to treat abnormal heart rhythms, or arrhythmias. They are important because they help regulate the heart's electrical system, ensuring the heart beats at a normal rhythm and preventing potentially life-threatening conditions.
What is the role of the sinoatrial (SA) node in the heart's electrical system?
-The SA node serves as the heart's natural pacemaker, initiating the electrical signals that cause the atria to contract and push blood into the ventricles. It is the starting point of the cardiac conduction system.
How does the cardiac conduction system consist of five elements?
-The cardiac conduction system is made up of the sinoatrial node (SA node), atrioventricular node (AV node), bundle of His, bundle branches, and Purkinje fibers. These elements work together to generate and transmit electrical signals for the heart's contractions.
What is the significance of the P wave, Q wave, R wave, S wave, and T wave on an electrocardiogram (ECG)?
-The P wave on an ECG represents atrial depolarization and the beginning of atrial contraction. The Q wave indicates the start of ventricular depolarization. The R wave is the peak of ventricular depolarization, the S wave follows and represents the end of depolarization. Lastly, the T wave represents the recovery phase of the ventricles as they repolarize.
What are the two types of cardiac cells and their functions?
-There are contractile cells, which generate force for heart contractions and make up most of the atrial and ventricular walls, and conducting cells, which initiate the electrical impulses controlling heart contractions.
What is automaticity and why is it important in the heart?
-Automaticity is the ability of certain cardiac cells, particularly in the SA node, AV node, bundle of His, and Purkinje fibers, to spontaneously initiate an action potential. It is important because it allows the heart to maintain a regular rhythm without external stimulation.
What are the three basic mechanisms responsible for the initiation of tachyarrhythmias?
-The three mechanisms are abnormal automaticity, triggered activity, and reentry. Abnormal automaticity occurs when cells become more permeable to sodium, leading to increased automaticity. Triggered activity involves abnormal leakage of positive ions causing afterdepolarizations. Reentry is a loop of electrical activation circulating through heart tissue, often due to an accessory pathway.
How does the Vaughan Williams classification categorize antiarrhythmic drugs?
-The Vaughan Williams classification divides antiarrhythmic drugs into four classes based on their dominant mechanism of action: Class 1 (sodium channel blockers), Class 2 (beta blockers), Class 3 (potassium channel blockers), and Class 4 (calcium channel blockers).
What are the potential adverse effects of class 1 antiarrhythmic drugs?
-Class 1 antiarrhythmic drugs can cause adverse effects such as blurred vision, headache, tinnitus, and in some cases, they may even cause arrhythmias themselves. The specific side effects can vary depending on the drug within this class.
How do class 2 antiarrhythmic drugs, such as beta blockers, affect the heart?
-Class 2 antiarrhythmic drugs, which are beta blockers, work by acting on beta-1 receptors to prevent the action of catecholamines on the heart. This results in decreased heart rate, reduced contractility, and slowed conduction through the AV node.
What is unique about sotalol among class 3 antiarrhythmic drugs?
-Sotalol is unique because it has both potassium channel blocking activity, like other class 3 drugs, and beta receptor blocking activity. This dual mechanism makes it effective for treating certain types of arrhythmias.
How does Digoxin work and what are its main uses?
-Digoxin works by inhibiting the sodium-potassium pump, leading to increased intracellular calcium which enhances myocardial contractility. It also stimulates the parasympathetic system, slowing sinus node discharge rate and AV node conduction. It is used particularly for patients with heart failure and atrial fibrillation.
What is the primary indication for Adenosine and what are its common side effects?
-Adenosine is primarily indicated for the acute treatment of supraventricular tachycardia. Its common side effects include chest pain, flushing, and hypotension due to its very short duration of action and need for IV administration.
What is the role of Magnesium Sulfate in treating arrhythmias?
-Magnesium Sulfate is effective for treating certain types of arrhythmias, such as torsades de pointes and those induced by Digoxin. Its precise mechanism is not fully understood, but it is known to play a role in the transport of sodium, potassium, and calcium across cell membranes.
Outlines

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraMindmap

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraKeywords

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraHighlights

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraTranscripts

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraVer Más Videos Relacionados

Guyton and Hall Medical Physiology (Chapter 10) REVIEW Cardiac Conductive Tissue || Study This!

BIOLOGI Kelas 11 - Sistem Peredaran Darah (PART 2) | GIA Academy

How the Heart Works (Animation)

BL DISTUM - Iacoviello - Lezione 2 - Principi di elettrofisiologia
Pharmacology – HEART FAILURE (MADE EASY)

Sistema Cardiovascular 6/6: Atividade elétrica do coração | Anatomia e etc.
5.0 / 5 (0 votes)
