Advanced EKGs - The Subtypes of Atrial Flutter (typical vs. reverse typical vs. atypical)
Summary
TLDRThis advanced EKG video explores the subtypes of atrial flutter, assuming basic knowledge of flutter and reentry mechanisms. It provides a detailed explanation of the right atrial anatomy and how it relates to atrial flutter, including the role of the caveo-tricuspid isthmus in creating reentrant circuits. The video discusses the major subtypes of atrial flutter, such as typical counterclockwise, reverse typical (clockwise), and isthmus-independent flutter, with a focus on their EKG characteristics. The video also touches on the challenges in diagnosing and mapping isthmus-independent flutters, and the limitations of traditional EKG definitions of atrial flutter.
Takeaways
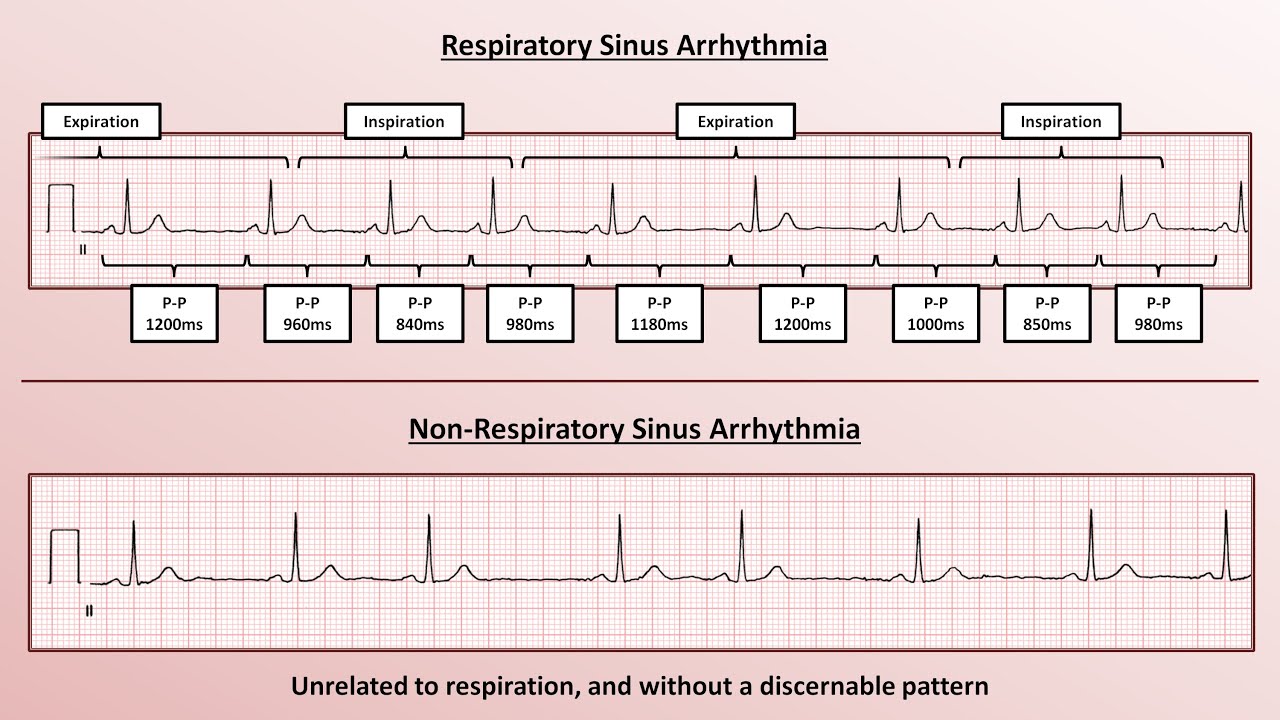
- 😀 Atrial flutter is defined by a rhythm with regular atrial activity, at least 240 flutter waves per minute, and an absence of an isoelectric baseline in at least one EKG lead.
- 😀 Atrial flutter typically involves a macroscopic reentry circuit within the right atrium.
- 😀 The right atrium is divided into two halves: the anterior lateral trabeculae and the smooth-walled posterior medial half.
- 😀 The caveo-tricuspid isthmus (CTI) is a key region in atrial flutter, where slowed conduction and anatomical barriers create a substrate for reentry circuits.
- 😀 The most common form of atrial flutter involves a counterclockwise reentry circuit around the CTI.
- 😀 Atrial flutter can also occur in reverse (clockwise) direction, known as reverse typical flutter.
- 😀 There are other rare forms of atrial flutter, such as lower loop reentry, which involves the IBC and the right atrium.
- 😀 Atrial flutter can be categorized into isthmus-dependent and isthmus-independent subtypes. The former is easier to treat with ablation.
- 😀 Typical counterclockwise flutter is identified by sawtooth flutter waves in the inferior leads and a positive isoelectric segment in V1.
- 😀 Isthmus-independent flutter is more variable, and it can resemble a wide range of patterns, from typical flutter to atrial tachycardia.
- 😀 EKG features alone are not always predictive of the exact location of reentry circuits, particularly for isthmus-independent flutters.
Q & A
What is the primary physiological mechanism behind atrial flutter?
-Atrial flutter is primarily caused by a macroscopic reentry circuit within one of the atria, typically the right atrium. This reentry circuit leads to rapid, regular atrial depolarization.
How is atrial flutter traditionally defined on an EKG?
-Atrial flutter is traditionally defined by the following criteria: regular atrial rhythm with at least 240 flutter waves per minute, absence of an isoelectric baseline in at least one lead, and a macro reentrant circuit in the atrium.
What anatomical structures are crucial in the development of atrial flutter?
-The right atrial anatomy is essential, particularly the cave o tricuspid isthmus (CTI), which plays a key role in the slow conduction of electrical impulses that form the reentry circuit. Other structures include the superior and inferior vena cava and the tricuspid valve.
What is the cave o tricuspid isthmus, and why is it important in atrial flutter?
-The cave o tricuspid isthmus (CTI) is a region of tissue between the tricuspid annulus and the eustachian ridge. It is important because electrical impulses can travel unusually slowly through this area, contributing to the formation of a reentry circuit, which is common in atrial flutter.
What is the main distinction between isthmus-dependent and isthmus-independent atrial flutter?
-Isthmus-dependent flutter involves a reentry circuit that passes through the CTI, while isthmus-independent flutter involves circuits that do not pass through the CTI and can occur in either the right or left atrium.
How can atrial flutter be categorized by cardiologists?
-Cardiologists categorize atrial flutter based on whether the reentry circuit is isthmus-dependent (passing through the CTI) or isthmus-independent (occurring around other anatomical barriers). The most common isthmus-dependent flutter is the counterclockwise or typical flutter.
What are the key EKG characteristics of typical counterclockwise atrial flutter?
-Typical counterclockwise flutter shows characteristic sawtooth waves, particularly in the inferior leads. These waves have a steep upstroke and shallow downstroke, with a well-defined isoelectric segment in lead V1 that separates rapid positive waveforms.
How does reverse typical or clockwise flutter appear on an EKG?
-In reverse typical flutter, the EKG shows positive, often notched flutter waves in the inferior leads and negative, broad waves in lead V1. The pattern reflects a reversal of the typical depolarization direction in the right atrium.
What is lower loop reentry, and how does it affect the EKG?
-Lower loop reentry occurs when the reentry circuit involves the inferior vena cava (IVC), with depolarization traveling around the IVC. The EKG can show negative atrial complexes in the inferior leads but may resemble typical or reverse typical flutter depending on the circuit's location.
How do isthmus-independent flutters differ in their EKG patterns?
-Isthmus-independent flutters show highly variable EKG patterns. They can resemble typical flutter, reverse typical flutter, or atrial tachycardia. The key difference is that these circuits do not use the CTI, making their classification more complex.
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级5.0 / 5 (0 votes)