Chronic kidney disease: Clinical Nursing Care
Summary
TLDRChronic Kidney Disease (CKD) is a progressive and irreversible condition marked by a decline in kidney function, evidenced by a reduced glomerular filtration rate (GFR). It can result from conditions like diabetes, hypertension, or kidney infections. Symptoms are often silent, with damage leading to fluid retention, toxin buildup, and complications across multiple organ systems. Treatment focuses on managing fluid and electrolyte balance, slowing disease progression, and addressing complications. Education for patients includes lifestyle changes, proper medication adherence, and monitoring signs like weight gain or changes in urine, with regular follow-ups essential for managing CKD effectively.
Takeaways
- 😀 Chronic Kidney Disease (CKD) is a condition characterized by a slow and progressive decrease in kidney function, with a GFR of less than 60 mL/min over at least three months.
- 😀 The kidneys function as natural blood filters, clearing metabolic waste and toxins, regulating pH, blood pressure, and electrolytes, and secreting important hormones.
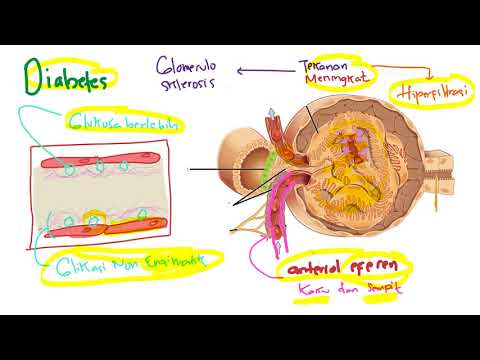
- 😀 CKD is often caused by conditions like diabetes mellitus and hypertension, with other causes including renal artery stenosis, polycystic kidney disease, and systemic disorders like lupus.
- 😀 Risk factors for CKD include obesity, cardiovascular disease, uncontrolled diabetes, smoking, and exposure to nephrotoxic medications.
- 😀 CKD is classified into five stages based on the estimated GFR, with stage 5 indicating complete kidney failure requiring renal replacement therapy.
- 😀 Symptoms of CKD can include fatigue, nausea, loss of appetite, fluid retention, and electrolyte imbalances like hyperkalemia.
- 😀 Diagnosis of CKD involves blood tests showing increased creatinine and BUN, urine analysis for proteinuria, hematuria, and ultrasound for kidney damage.
- 😀 Treatment for CKD involves managing blood pressure, blood glucose levels, and preventing complications such as proteinuria, hypertension, and anemia.
- 😀 In later stages (stage 3 and above), additional treatments may include dialysis, kidney transplantation, and managing bone health with calcium and phosphate supplementation.
- 😀 Nursing care for CKD patients includes monitoring fluid status, electrolytes, and vital signs, providing education on lifestyle changes, and ensuring medication adherence and safe self-management.
Q & A
What is Chronic Kidney Disease (CKD) and how is it defined?
-Chronic Kidney Disease (CKD) is a condition where kidney function progressively declines over time. It is characterized by a glomerular filtration rate (GFR) of less than 60 milliliters per minute, persisting for at least 3 months.
How do the kidneys function and what is their role in the body?
-The kidneys filter the blood, removing metabolic waste and toxins, and excrete them as urine. They also regulate electrolyte balance, blood pressure, acid-base balance, and secrete important hormones.
What are the main causes of CKD in the United States?
-The leading causes of CKD in the United States are diabetes mellitus and hypertension. Other causes include renal artery stenosis, polycystic kidney disease, and systemic conditions like lupus.
How is CKD classified and what are the stages?
-CKD is classified into five stages based on GFR: Stage 1 (normal function, GFR ≥90), Stage 2 (mild decrease, GFR 60-89), Stage 3 (moderate decrease, GFR 30-59), Stage 4 (severe decrease, GFR 15-29), and Stage 5 (end-stage kidney disease, GFR <15).
What are the symptoms of CKD as it progresses?
-As CKD progresses, symptoms like polyuria, nocturia, and edema may appear. Fluid retention can lead to oliguria, and waste buildup (uremia) can cause fatigue, nausea, and loss of appetite. Serious complications may affect multiple body systems.
What laboratory tests are used to diagnose CKD?
-Diagnosis of CKD involves blood tests showing elevated creatinine and urea levels, a decreased GFR, and a urine analysis showing proteinuria, hematuria, or abnormal cells. Imaging such as ultrasound may also be done.
What treatments are recommended in the early stages of CKD?
-In early stages (1-2), treatment focuses on slowing disease progression through lifestyle changes like smoking cessation, controlling blood pressure and blood glucose, and avoiding nephrotoxic medications. Medications like ACE inhibitors or ARBs may be used to manage hypertension and proteinuria.
How is anemia treated in patients with CKD?
-Anemia in CKD patients is typically treated by addressing the underlying cause, such as managing erythropoiesis with erythropoietin-stimulating agents and iron supplements. Blood transfusions may also be considered in severe cases.
What is renal osteodystrophy and how is it managed?
-Renal osteodystrophy is a condition where bones become weak and brittle due to abnormal calcium and phosphate metabolism in CKD. It is managed through calcium and phosphate binders, vitamin D supplements, and ensuring proper nutrition.
What is the role of nurses in the care of CKD patients?
-Nurses monitor fluid and electrolyte balance, assess vital signs, and track weight changes. They also administer prescribed medications, educate patients about lifestyle modifications, and prepare them for renal replacement therapy as needed. Emotional support is also crucial for patient adjustment.
Outlines

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードMindmap

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードKeywords

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードHighlights

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードTranscripts

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレード関連動画をさらに表示
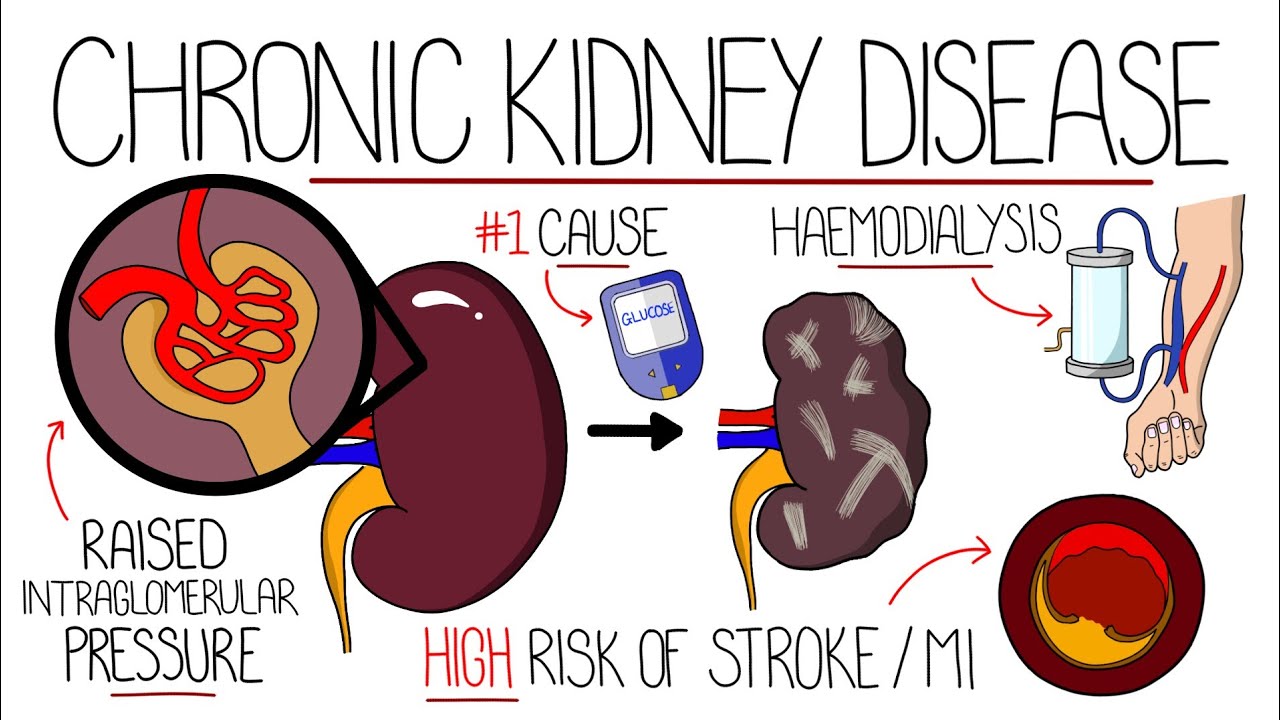
Understanding Chronic Kidney Disease (CKD)
No KIDNEY Patient Will Ever Lose a Kidney Again (Thanks To This 6 Tips)
Chronic kidney disease - causes, symptoms, diagnosis, treatment, pathology
Chronic Renal Failure (Chronic Kidney Disease) ESRD l Nursing NCLEX RN & LPN
Patofisiologi - Penyakit Ginjal Kronis (PGK) / Chronic kidney disease (CKD)

Part 3 - Primary Care Insights from the KDIGO 2024 CKD Guideline: Staging of CKD
5.0 / 5 (0 votes)
