Bronchodilators Part 2: Mechanisms of Action
Summary
TLDRThis video explains the mechanisms of action of bronchodilators, focusing on beta-2 adrenoceptor agonists like salbutamol and muscarinic receptor antagonists such as tiotropium bromide. It details how these drugs relax smooth muscle cells in the airways by altering intracellular signaling, including G protein-coupled receptor pathways. For beta-2 agonists, increased cAMP and myosin phosphatase activation lead to muscle relaxation, while muscarinic antagonists block acetylcholine, reducing muscle contraction. This comprehensive guide covers key pharmacological strategies used in treating pulmonary diseases.
Takeaways
- 😀 Salbutamol (albuterol) is the most commonly used bronchodilator, primarily administered via inhalation for fast and selective delivery to the lungs.
- 😀 Beta-2 adrenergic agonists, like salbutamol, activate the Gαs signaling pathway, leading to increased cAMP levels in smooth muscle cells.
- 😀 Elevated cAMP activates protein kinase A (PKA), which promotes the dephosphorylation of myosin light chain (MLC) by activating myosin phosphatase.
- 😀 Dephosphorylated myosin light chain reduces myosin-actin interaction, leading to smooth muscle relaxation and bronchodilation.
- 😀 The dissociation of the Gβ/Gγ dimer from the G protein heterotrimer activates potassium channels, resulting in hyperpolarization and reduced calcium ion mobilization.
- 😀 Lower calcium mobilization further inhibits smooth muscle contraction, contributing to bronchodilation.
- 😀 Muscarinic receptor antagonists, such as tiotropium bromide, block acetylcholine's action on M3 muscarinic receptors, leading to reduced smooth muscle contraction.
- 😀 Muscarinic receptor activation triggers the Gαq pathway, which activates phospholipase C (PLC) and leads to the production of DAG and IP3.
- 😀 DAG activates protein kinase C (PKC), which inhibits myosin light chain phosphatase and promotes myosin light chain phosphorylation, enhancing contraction.
- 😀 Blocking acetylcholine from activating M3 receptors with muscarinic antagonists reduces the signaling for muscle contraction, enhancing bronchodilation.
Q & A
What is the primary purpose of bronchodilators in treating pulmonary diseases?
-Bronchodilators are used to reduce resistance to airflow in the airways by relaxing smooth muscle cells, which helps to treat conditions like asthma and chronic obstructive pulmonary disease (COPD).
How does salbutamol (albuterol) act as a bronchodilator?
-Salbutamol works by binding to beta-2 adrenoceptors on bronchial smooth muscle cells, which activates the Gαs signaling pathway, increasing cAMP levels and leading to smooth muscle relaxation.
Why is inhalation the preferred method of administering salbutamol?
-Inhalation delivers the drug directly to the lungs, ensuring fast action and greater tissue selectivity, as it targets the areas where airflow is restricted without passing through the bloodstream.
What role does cAMP play in the mechanism of action of beta-2 adrenoceptor agonists?
-cAMP activates protein kinase A (PKA), which in turn activates myosin phosphatase, leading to dephosphorylation of the myosin light chain, reducing contractility, and promoting smooth muscle relaxation.
What is the effect of Gβ/Gγ dissociation in beta-2 adrenoceptor signaling?
-The dissociation of Gβ/Gγ activates potassium channels, causing K+ efflux, hyperpolarizing the smooth muscle cell, which reduces calcium mobilization and further decreases muscle contraction.
What role does calcium play in smooth muscle contraction?
-Calcium ions bind to calmodulin, which then activates myosin light chain kinase, leading to the phosphorylation of the myosin light chain and promoting muscle contraction.
How does beta-2 adrenoceptor stimulation reduce intracellular calcium levels?
-Beta-2 adrenoceptor stimulation reduces calcium mobilization by activating the Gβ/Gγ dimer, which inhibits calcium release, thus leading to less calcium available for muscle contraction.
What is the mechanism of action of muscarinic receptor antagonists like tiotropium bromide?
-Muscarinic receptor antagonists block acetylcholine from activating M3 muscarinic receptors on bronchial smooth muscle cells. This prevents the Gαq pathway from stimulating calcium release and myosin light chain phosphorylation, leading to muscle relaxation.
What is the significance of the M3 muscarinic receptor in bronchodilation?
-M3 muscarinic receptors are the most prevalent on bronchial smooth muscle cells. When activated, they trigger the Gαq pathway, which increases intracellular calcium and promotes muscle contraction. Blocking these receptors leads to bronchodilation.
How do muscarinic receptor antagonists impact smooth muscle cell contraction?
-By blocking acetylcholine from binding to M3 receptors, muscarinic receptor antagonists reduce intracellular calcium levels and inhibit myosin light chain phosphorylation, leading to smoother muscle relaxation and bronchodilation.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Pharmacology - DRUGS FOR ASTHMA AND COPD (MADE EASY)
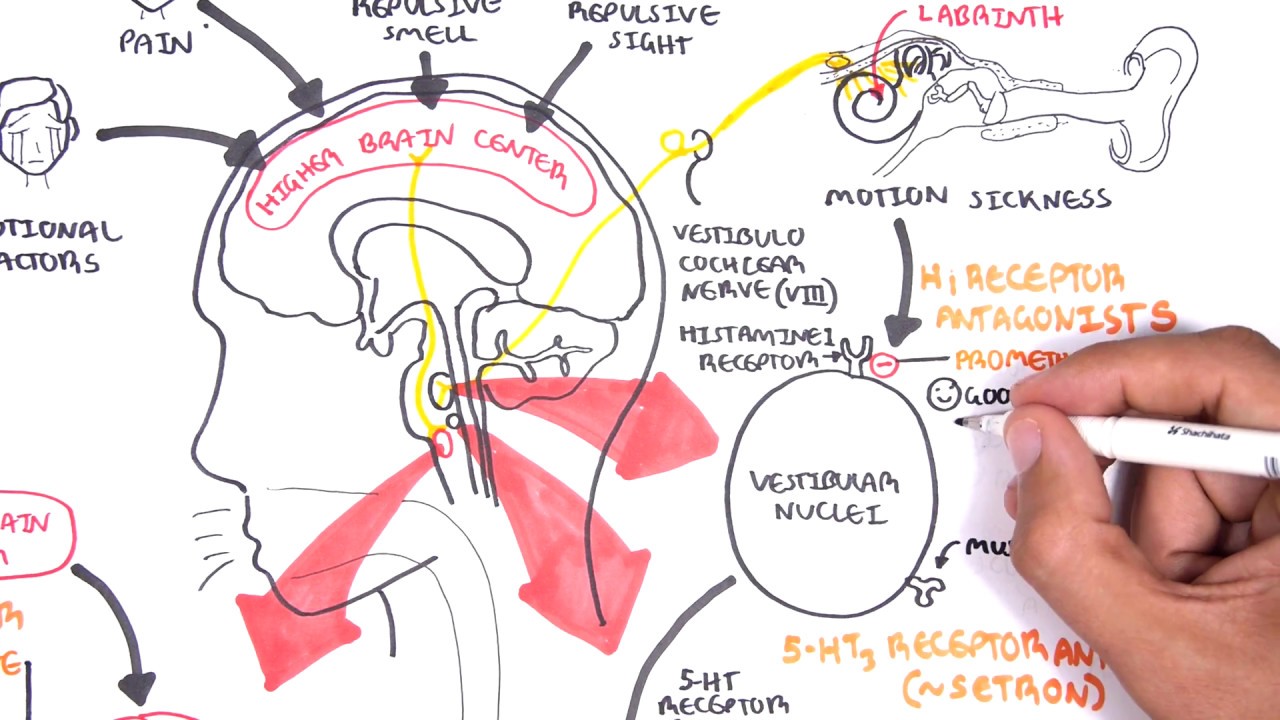
Pharmacology - Antiemetics

قیمت 4بخش2

Curso de Farmacologia: Aula 7 - Farmacologia adrenergica - Agonistas e antagonistas diretos

Agonistas Colinérgicos (Diretos/Muscarínicos) | Aula 10 | Farmacologia rápida e fácil | Flavonoide

Pharmacology MADE EASY (Drugs and Receptors) - Perfect for beginners
5.0 / 5 (0 votes)