Gestational Diabetes (Pregnancy Diabetes) | Causes, Risk Factors, Symptoms, Consequences, Treatment
Summary
TLDRThis lesson on gestational diabetes explains its pathophysiology, risk factors, diagnosis, and treatment. Gestational diabetes is a common condition that occurs during pregnancy, leading to insulin resistance and elevated glucose levels. The course covers the potential complications for both the mother, such as hypertension and preeclampsia, and the infant, including macrosomia and hypoglycemia. The lesson also outlines the screening process and the two main diagnostic methods. Management strategies include diet, exercise, and medications like insulin. Long-term risks for both mother and child include obesity, type 2 diabetes, and cardiovascular disease, highlighting the importance of early detection and care.
Takeaways
- 😀 Gestational diabetes (GDM) is a form of diabetes that develops during pregnancy, typically in the second or third trimester.
- 😀 GDM is caused by insulin resistance, where the body struggles to bring glucose into cells due to pregnancy hormones like human placental lactogen.
- 😀 There are two types of GDM: A1 (diet-controlled) and A2 (medication-controlled).
- 😀 Gestational diabetes affects about 2-10% of pregnancies in the U.S. and is linked to rising rates of obesity and diabetes.
- 😀 Risk factors for GDM include obesity (BMI >25), family history of type 2 diabetes, physical inactivity, and metabolic syndrome.
- 😀 High levels of glucose in the mother’s blood can lead to fetal hyperglycemia, causing the fetus to produce more insulin, leading to growth complications like macrosomia (large baby).
- 😀 Maternal complications of GDM include gestational hypertension, preeclampsia, and an increased risk for future type 2 diabetes, obesity, and cardiovascular diseases.
- 😀 Infants born to mothers with GDM are at risk for neonatal hypoglycemia, respiratory distress, hyperbilirubinemia (jaundice), and shoulder dystocia during delivery.
- 😀 Long-term effects for infants include a higher risk of obesity, ADHD, and neuropsychiatric conditions like autism and epilepsy.
- 😀 Diagnosis of GDM is typically done via a glucose tolerance test during pregnancy (24-28 weeks) using either a one-step or two-step approach.
- 😀 Treatment for GDM includes diet management, exercise, and if necessary, medications like insulin or oral agents, with a focus on controlling blood glucose levels during pregnancy.
Q & A
What is gestational diabetes and when does it occur?
-Gestational diabetes mellitus (GDM) is a condition where glucose intolerance is first identified during pregnancy, typically during the second or third trimester. It may also occur in patients who were previously undiagnosed with diabetes before pregnancy.
What are the two types of gestational diabetes?
-The two types of gestational diabetes are A1 and A2. A1 is controlled by diet, while A2 requires medication, such as insulin or oral medication, to regulate blood glucose levels.
What are the main risk factors for gestational diabetes?
-The main risk factors include being overweight or obese (BMI > 25), having a family history of type 2 diabetes, physical inactivity, high triglycerides, low HDL, abnormal glucose tolerance tests, polycystic ovary syndrome (PCOS), a past history of gestational diabetes, and older maternal age.
How does the placenta contribute to insulin resistance in gestational diabetes?
-The placenta produces human placental lactogen, which inhibits insulin action on its receptors, leading to insulin resistance. This, combined with other pregnancy hormones like prolactin, growth hormone, and progesterone, further exacerbates insulin resistance in the mother.
What are some short-term maternal complications of gestational diabetes?
-Some short-term complications for the pregnant mother include gestational hypertension, preeclampsia, weight gain beyond standard expectations, and an increased risk of developing gestational diabetes in subsequent pregnancies.
What are the potential effects on the infant of a mother with gestational diabetes?
-Infants may experience macrosomia (large body size), neonatal hypoglycemia, hyperbilirubinemia (leading to jaundice), respiratory distress, shoulder dystocia, and an increased risk of developing obesity or type 2 diabetes later in life.
What is macrosomia, and why is it a concern in infants born to mothers with gestational diabetes?
-Macrosomia refers to a large body size, typically over 4,000 grams. It is a concern because it can lead to complications during delivery, such as shoulder dystocia, and may result in long-term health issues for the infant, including an increased risk of obesity.
How does neonatal hypoglycemia occur in infants of mothers with gestational diabetes?
-Neonatal hypoglycemia occurs because the infant’s pancreas produces excess insulin in response to high glucose levels from the mother. After birth, the infant no longer receives the high glucose from the mother, but the high insulin levels continue, leading to a drop in the infant's blood glucose.
What are the long-term risks for the mother after having gestational diabetes?
-After delivery, mothers who had gestational diabetes are at an increased risk for developing type 2 diabetes (35-60% higher risk within 10-20 years), cardiovascular disease, certain types of cancer (such as ovarian, endometrial, and breast cancer), eye conditions, and kidney disease.
How is gestational diabetes diagnosed?
-Gestational diabetes can be diagnosed using either a one-step or two-step approach. The one-step approach involves a 75-gram oral glucose tolerance test, while the two-step approach includes an initial 50-gram glucose challenge test followed by a 100-gram test if necessary.
Outlines

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraMindmap

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraKeywords

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraHighlights

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraTranscripts

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraVer Más Videos Relacionados

Type 2 diabetes mellitus (mechanism of disease)

Anemia of Chronic Disease | Causes, Pathophysiology, Signs & Symptoms, Diagnosis, Treatment
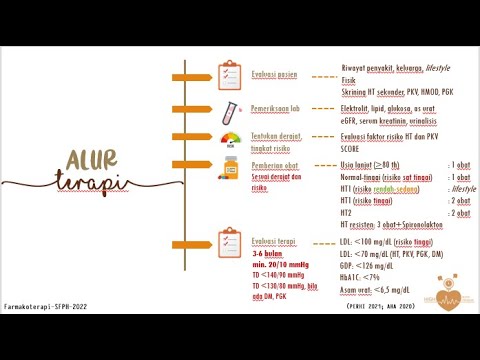
FARMAKOTERAPI HIPERTENSI TERBARU: Klasifikasi, Risiko (SCORE), Alur Terapi PERHI 2021, AHA 2020

DIABETES MELITUS (DM) tipe 2

Cancer: Pathophysiology, Risk Factors, Signs/Symptoms and more - Medical Surgical | @LevelUpRN

Preeklamsia Hipertensi Dalam Kehamilan - Patofisiologi, Diagnosis, Manajemen Persalinan dan Obat
5.0 / 5 (0 votes)
