Pulmonary 2 Lung Volumes and Ventilation
Summary
TLDRThis lecture delves into the mechanics of a spirometer, a device measuring lung volumes and capacities. It explains the traditional water displacement method and modern alternatives, and covers both static and dynamic lung function assessments. The importance of understanding lung volumes, such as vital capacity and total lung capacity, is highlighted, along with dynamic measures like forced vital capacity and maximum voluntary ventilation, crucial for diagnosing respiratory conditions. The lecture also touches on concepts like dead space and alveolar ventilation, essential for gas exchange efficiency.
Takeaways
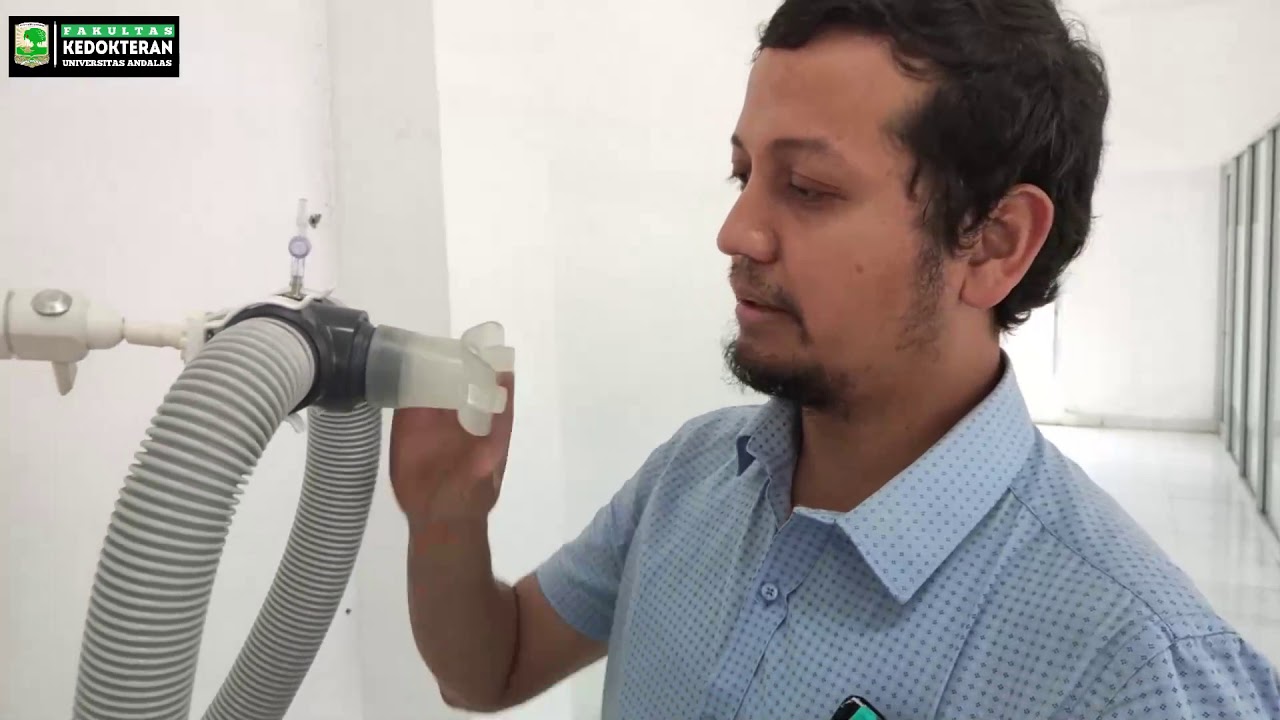
- 🌊 A spirometer is a device used to measure lung volumes and capacities, traditionally involving a water-filled chamber and a tube for breathing.
- 📏 The movement of air due to breathing causes the water level in the spirometer to rise and fall, which is directly proportional to the volume of air displaced.
- 📊 Lung volume measurements are calibrated using markers or scales on the spirometer for precise readings.
- 🚀 Modern spirometers have evolved to be smaller, with examples like turbine models and clinical ear displacement boxes.
- 🔍 Lung volumes can vary significantly based on factors such as age, gender, body size, and height.
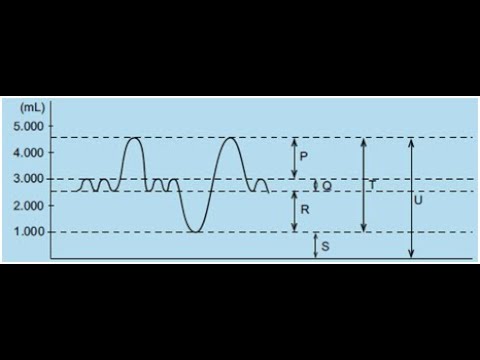
- 🏗️ Static lung volume tests measure the dimensional aspects of air movement without time limitations, providing a snapshot of lung volume.
- 🌪️ Dynamic lung volume tests assess air movement over time, focusing on expiratory power and resistance to air movement in the lungs.
- 📉 The ratio of forced expired volume in 1 second to forced vital capacity (FEV1/FVC) is a key dynamic measure, with lower ratios indicating potential lung obstruction.
- 🏋️♂️ Maximum voluntary ventilation (MVV) measures the maximum volume of air a person can breathe in one minute, with elite athletes showing remarkably high values.
- 🌀 Dead space refers to the portion of the respiratory tract where gas exchange does not occur, including both anatomic and physiological dead spaces.
- 🔄 Alveolar ventilation is the portion of minute ventilation that reaches the alveoli for gas exchange, affected by the presence of dead space.
Q & A
What is a spirometer and what is its primary function?
-A spirometer is a device used to measure lung volumes and capacities in respiratory physiology. It operates by having a subject breathe in and out through a tube connected to a chamber filled with water. The fluctuation in water level, which is proportional to the volume of air displaced, is used to measure lung function.
How are the markers or scales on a spirometer used?
-The markers or scales on a spirometer are calibrated to specific volume measurements, allowing for precise readings of the water level changes. This enables researchers and clinicians to quantify various lung parameters with accuracy.
What are the two types of measurements used to assess lung volumes and capacities?
-The two types of measurements used to assess lung volumes and capacities are static and dynamic measurements. Static lung volume tests focus on the dimensional aspects of air movement within the pulmonary tract without time limitation, while dynamic tests assess expiratory power and resistance to air movement in the lungs.
What is the significance of the forced vital capacity (FVC) in lung function testing?
-The forced vital capacity (FVC) represents the total lung volume moved in one breath from full inspiration to maximum expiration. It is a crucial measure in lung function testing as it provides insights into the overall lung capacity and can indicate the presence of respiratory conditions.
How does the forced expiratory volume in 1 second (FEV1) relate to FVC and why is it important?
-The FEV1 is the volume of air expired during the first second of a forced vital capacity maneuver. The ratio of FEV1 to FVC is important as it provides diagnostic insights into expiratory power and resistance in the lungs. A decreased ratio can indicate conditions like severe obstructive pulmonary disease or asthma.
What is the maximum voluntary ventilation (MVV) and how is it measured?
-The maximum voluntary ventilation (MVV) is the volume of air breathed during rapid and deep breathing for 15 seconds, multiplied by four to represent the volume breathed for 1 minute. It is an assessment of ventilatory capacity and can vary significantly among individuals, including elite athletes.
What is the role of the tidal volume in respiratory physiology?
-Tidal volume refers to the volume of air moved during either the inspiratory or expiratory phase of each breathing cycle under resting conditions. It is a key parameter in understanding the efficiency of the respiratory system and gas exchange.
What is the significance of the residual lung volume (RLV) in lung function?
-The residual lung volume (RLV) is the volume of air that remains in the lungs after maximal exhalation. It contributes to the total lung capacity and can be affected by various factors, including the individual's height and potential genetic influences.
What is meant by 'anatomic dead space' in the respiratory tract?
-Anatomic dead space refers to the portion of the respiratory tract, such as the nose, mouth, and trachea, where air remains and does not participate in gas exchange. It is a part of the total volume of air inhaled but does not contribute to alveolar ventilation.
How does physiological dead space differ from anatomic dead space?
-Physiological dead space refers to the portion of alveolar volume with poor tissue perfusion or inadequate ventilation, which does not participate in gas exchange. Unlike anatomic dead space, physiological dead space can increase significantly in certain conditions due to inadequate perfusion or ventilation.
What factors can affect the efficiency of alveolar ventilation?
-Factors that can affect the efficiency of alveolar ventilation include the presence of dead space, the depth of breathing, and the individual's overall lung function. Efficient alveolar ventilation is crucial for maintaining consistent alveolar air composition and stable arterial blood gases.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video
5.0 / 5 (0 votes)