IMAT Biology Lesson 6.6 | Anatomy and Physiology | Respiratory System
Summary
TLDRIn this detailed lecture on the human respiratory system, Andre explores the anatomy and physiology of both the upper and lower respiratory tracts. He explains key structures like the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles, and alveoli, emphasizing their roles in gas exchange. The lecture covers the mechanics of breathing, including muscle involvement and pressure changes, and introduces lung volumes and capacities measured by spirometry. Finally, Andre touches on how gases like oxygen and carbon dioxide are transported in the blood, laying the foundation for understanding respiratory and circulatory system diseases.
Takeaways
- 🧠 Introduction to the anatomy and physiology of the human respiratory system.
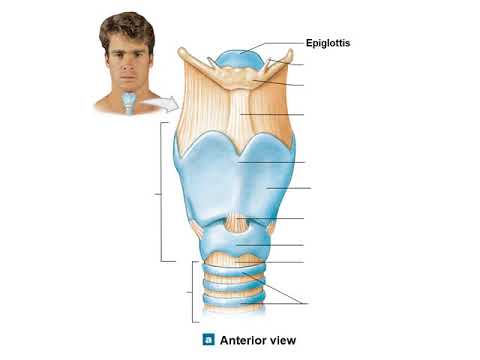
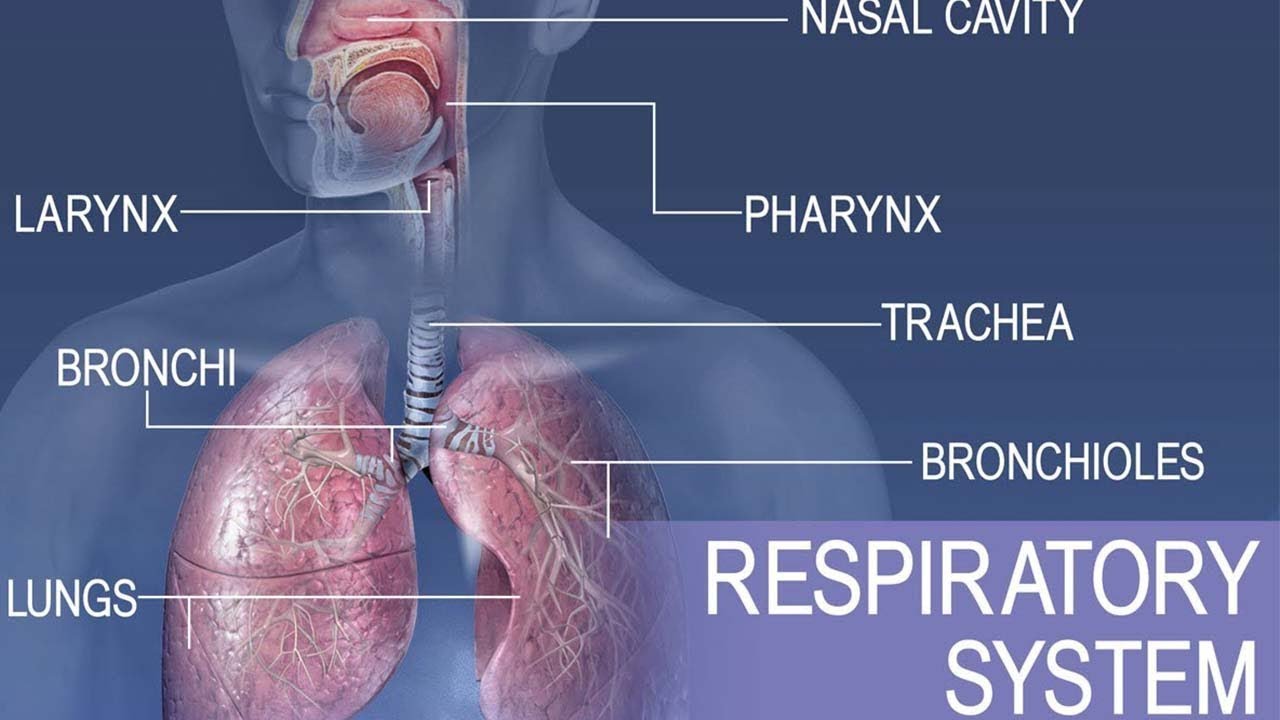
- 👃 The upper respiratory tract includes the nasal cavity, pharynx, and larynx, which contains the vocal cords.
- 🔄 The lower respiratory tract begins with the trachea, which splits into the primary bronchi leading to the lungs.
- 🌬️ The bronchi divide into smaller tubes called terminal bronchioles, which further divide into respiratory bronchioles and alveolar ducts ending in alveoli where gas exchange occurs.
- 🫁 The diaphragm and intercostal muscles are crucial for lung contraction and expansion, facilitating breathing.
- 💨 Gas exchange occurs in the alveoli through diffusion, driven by differences in partial pressures of oxygen and carbon dioxide between alveoli and capillaries.
- 🦠 The trachea and bronchi have cartilage and goblet cells that produce mucus, helping trap and expel pathogens.
- 💪 Smooth muscles in the trachea and bronchi can contract to adjust airflow, responding to environmental conditions or allergic reactions.
- 🔍 Gas transport in the blood: Oxygen is carried by hemoglobin, while carbon dioxide is mostly transported as hydrogen carbonate in the plasma.
- 📉 Spirometry measures lung volumes and capacities, including tidal volume, vital capacity, and residual volume, which are critical for understanding respiratory health.
Q & A
What is the primary function of the nasal cavity in the respiratory system?
-The primary function of the nasal cavity is to filter, warm, and humidify the air we breathe in.
What are the main anatomical structures of the upper respiratory tract?
-The main anatomical structures of the upper respiratory tract include the nasal cavity, pharynx, and larynx.
What is the role of the trachea in the respiratory system?
-The trachea serves as a passage for air to travel from the upper respiratory tract to the lower respiratory tract and is supported by cartilage to keep it open.
Describe the pathway of air from the trachea to the alveoli.
-Air travels from the trachea to the primary bronchi, then to the terminal bronchioles, respiratory bronchioles, alveolar ducts, and finally reaches the alveoli where gas exchange occurs.
What is the function of the diaphragm in respiration?
-The diaphragm contracts and flattens to increase the volume of the thoracic cavity, reducing the pressure and allowing air to flow into the lungs. It relaxes to help expel air during exhalation.
How does gas exchange occur in the alveoli?
-Gas exchange occurs in the alveoli through diffusion, where oxygen moves from the alveoli into the blood in the capillaries, and carbon dioxide moves from the blood in the capillaries into the alveoli.
What are goblet cells and what is their function in the respiratory system?
-Goblet cells are cells that produce mucus to trap viruses, bacteria, and other particles, preventing them from entering the lungs and causing infection.
What is the difference between the right and left lungs in terms of lobes?
-The right lung has three lobes, while the left lung has two lobes.
Explain the concept of partial pressure in the context of gas exchange.
-Partial pressure refers to the pressure exerted by a specific gas in a mixture of gases. Gas exchange occurs because gases move from areas of higher partial pressure to areas of lower partial pressure.
What happens during anaphylactic shock in the respiratory system?
-During anaphylactic shock, the smooth muscles in the trachea and bronchus contract, narrowing the airways and making breathing difficult.
What is the function of the cilia in the respiratory system?
-Cilia are tiny hair-like projections that move mucus and trapped particles out of the respiratory tract, helping to keep the airways clear.
What are the different volumes and capacities measured in a spirogram?
-A spirogram measures tidal volume (normal breathing volume), total lung capacity, residual volume (air left in lungs after exhalation), functional residual capacity (residual volume plus expiratory reserve volume), inspiratory reserve volume, expiratory reserve volume, and vital capacity (inspiratory reserve volume plus tidal volume plus expiratory reserve volume).
How is carbon dioxide transported in the blood?
-Carbon dioxide is transported in the blood in three main ways: dissolved in plasma (5%), as hydrogen carbonate (85%) after combining with water and an enzyme, and as carbaminohemoglobin (10%) after combining with hemoglobin.
What is the significance of the pleural cavity in the respiratory system?
-The pleural cavity, the space between the parietal and visceral pleura, contains a small amount of fluid that reduces friction during breathing and helps maintain the negative pressure needed for lung expansion.
What happens to intrapleural pressure during inspiration?
-During inspiration, the intrapleural pressure decreases as the thoracic cavity volume increases, allowing air to flow into the lungs.
What is the relationship between volume and pressure in the lungs?
-Volume and pressure in the lungs are inversely related; increasing the volume of the lungs decreases the pressure, and decreasing the volume increases the pressure, facilitating the movement of air in and out of the lungs.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video
LESSON 1: Medical Surgical Nursing Respiratory System Introduction Supplemental Lecture

FISIOLOGI PERNAFASAN 1 | Yuk review kembali fisiologi pernafasan pada manusia
Anatomi Sistem Respirasi | Materi Kedokteran Dasar

Airway Anatomy - 3D Tutorial
Anatomy and physiology of Respiratory system

SISTEM PERNAPASAN MANUSIA PART 3 (GANGGUAN PADA SISTEM PERNAPASAN)
5.0 / 5 (0 votes)