Advanced EKGs - Sudden Cardiac Death (Hypertrophic cardiomyopathy, ARVD, Brugada syndrome, and CPVT)
Summary
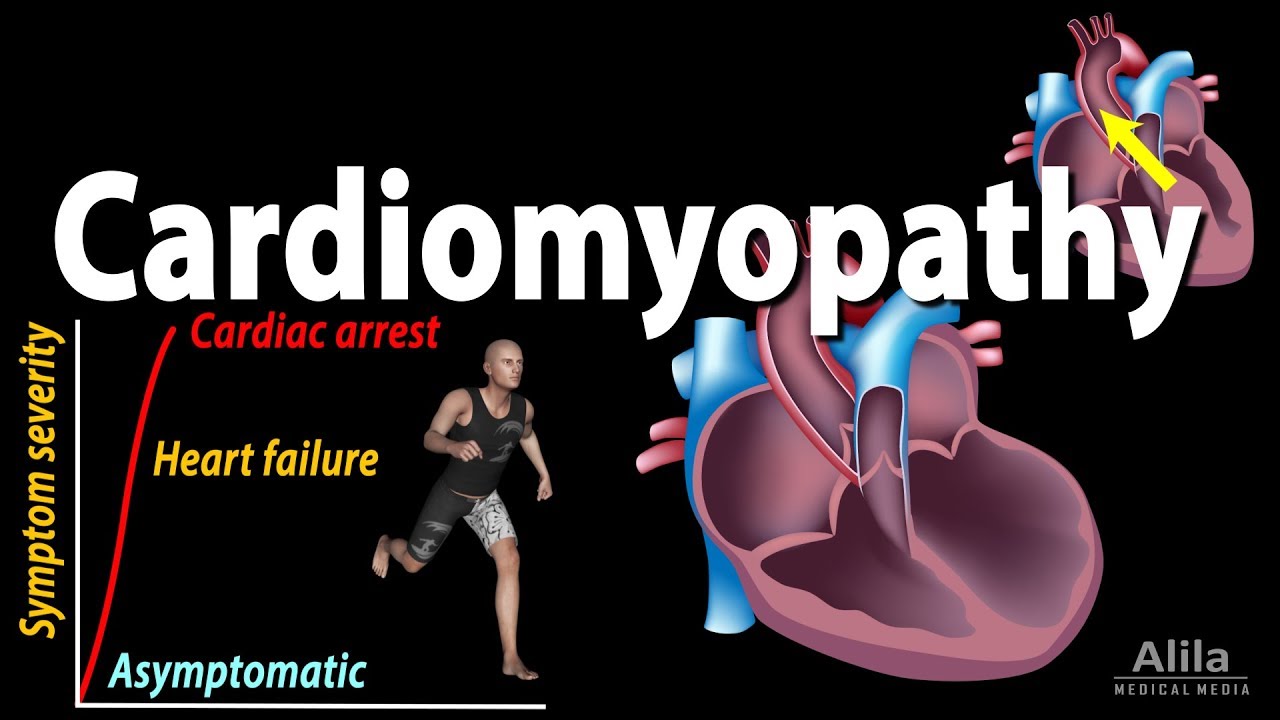
TLDRThis video from Stanford University explores the serious topic of sudden cardiac death and four rhythmogenic syndromes: hypertrophic cardiomyopathy (HCM), arrhythmogenic right ventricular dysplasia (ARVD), Brugada syndrome, and catecholaminergic polymorphic ventricular tachycardia (CPVT). The video dives into the pathogenesis, genetics, and EKG characteristics of these diseases, highlighting their potential to cause sudden cardiac arrest and death. Key features such as the unique EKG patterns, genetic factors, and risk of ventricular arrhythmias are discussed, providing valuable insights for understanding these life-threatening conditions and their impact on young athletes and the general population.
Takeaways
- 😀 Sudden cardiac arrest and sudden cardiac death occur when cardiac activity stops abruptly, leading to potential death or revival, with athletes being commonly affected.
- 😀 Sudden unexpected nocturnal death syndrome (SUND) describes unexplained deaths during sleep in young men from Southeast Asia, with possible associations to heart conditions like arrhythmias.
- 😀 Most cases of sudden cardiac death are caused by myocardial diseases (90%), while less than 10% are related to electrical processes of the heart.
- 😀 Hypertrophic cardiomyopathy (HCM) is a genetic heart disease that causes left ventricular hypertrophy and can result in sudden cardiac death, especially in athletes.
- 😀 Common EKG signs of hypertrophic cardiomyopathy include deep and narrow Q waves in the lateral and inferior leads, and inverted T-waves in the apical variant.
- 😀 Arrhythmogenic right ventricular dysplasia (ARVD) involves the replacement of myocardium with fibro-fatty tissue, leading to ventricular arrhythmias, with a key EKG feature being the Epsilon wave.
- 😀 Bugata syndrome is a relatively newly identified condition characterized by polymorphic ventricular tachycardia (VT) and sudden cardiac death, usually at rest or during sleep.
- 😀 The EKG patterns in Bugata syndrome are distinctive, with Type 1 presenting with downsloping ST elevations leading into inverted T-waves in V1 and V2, while Type 2 has a saddleback ST elevation.
- 😀 Catecholaminergic polymorphic ventricular tachycardia (CPVT) is caused by defective calcium handling in the sarcoplasmic reticulum, leading to exertion-induced polymorphic VT and sudden death.
- 😀 The key difference between the syndromes and patterns discussed (e.g., Bugata syndrome vs. pattern) lies in the presence of symptoms and risk factors such as sudden death or family history.
Q & A
What is the difference between sudden cardiac arrest and sudden cardiac death?
-Sudden cardiac arrest occurs when cardiac activity abruptly stops, but the patient can be revived. Sudden cardiac death refers to when the patient dies as a result of the cardiac arrest.
What is the significance of sudden unexpected nocturnal death syndrome (SUNDS)?
-SUNDS is a phenomenon where people die suddenly in their sleep without warning or explanation. It is particularly common in young, healthy men from Southeast Asia, including the Philippines, and is associated with agonal breathing and convulsions.
What are the most common causes of sudden cardiac death?
-Over 90% of cases are caused by primary myocardial processes, such as acquired structural heart disease, cardiomyopathies, and congenital heart disease. Less than 10% are due to primary electrical processes like channelopathies.
What is hypertrophic cardiomyopathy (HCM) and its genetic cause?
-HCM is a genetic disease of the myocardium that results in various forms of left ventricular hypertrophy, particularly septal hypertrophy. It is caused by mutations in contractile proteins, such as myosin and troponin, and is inherited in an autosomal dominant manner.
What are the EKG findings in hypertrophic cardiomyopathy?
-Typical EKG findings in HCM include deep and narrow Q waves in the lateral and inferior leads, indicating septal hypertrophy, and generalized signs of left ventricular hypertrophy (LVH). In the apical variant, there can be deeply inverted T waves in the precordial leads.
What is arrhythmogenic right ventricular dysplasia (ARVD) and its genetic cause?
-ARVD is a condition where the myocardium is replaced by fibro-fatty tissue, leading to arrhythmias. It is typically caused by mutations in desmosomal proteins and is inherited in an autosomal dominant fashion.
What is the key EKG finding in arrhythmogenic right ventricular dysplasia (ARVD)?
-The key EKG finding in ARVD is the presence of an Epsilon wave, a tiny positive deflection at the end of the QRS complex, particularly in the precordial leads V1-V3. Other findings may include a right bundle branch block and prolonged QRS duration.
What is Bugata syndrome and its association with sudden cardiac death?
-Bugata syndrome is a condition that leads to polymorphic ventricular tachycardia (VT) and ventricular fibrillation (VF), typically at rest or during sleep. It is associated with mutations in the SCN5A gene, which affects the cardiac sodium channel. It has been linked to sudden cardiac death, particularly in middle-aged men.
What are the distinctive EKG patterns in Bugata syndrome?
-Bugata syndrome has two distinct EKG patterns: Type 1 shows downsloping ST elevation with prominent T-wave inversions in leads V1 and V2, while Type 2 shows ST elevation with a saddleback configuration and upright or biphasic T-waves. Type 1 carries a higher risk of arrhythmias and death.
What is catecholaminergic polymorphic ventricular tachycardia (CPVT) and its genetic cause?
-CPVT is a condition characterized by recurrent polymorphic VT triggered by physical or emotional stress in the absence of structural heart disease. It is caused by mutations in genes that affect calcium handling in cardiac myocytes, particularly in the sarcoplasmic reticulum.
What are the EKG characteristics of catecholaminergic polymorphic ventricular tachycardia (CPVT)?
-In CPVT, the baseline EKG is usually normal. When polymorphic VT occurs, it may appear as typical polymorphic VT or as bidirectional VT, where the QRS complexes alternate between two distinct morphologies.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade Now5.0 / 5 (0 votes)