How to Perform Orthostatic Hypotension Testing
Summary
TLDRThe video explains how to conduct an orthostatic hypotension test, used to assess a patient's heart function, vasoconstriction, and hydration status. The procedure involves checking blood pressure in three different positions: laying down, sitting, and standing. The test measures compensatory mechanisms like vasoconstriction and heart rate adjustments in response to blood pooling. A significant drop in blood pressure or an abnormal heart rate increase may indicate underlying health issues such as dehydration or improper vasoconstriction. The video emphasizes the importance of understanding these physiological responses and their implications.
Takeaways
- 😀 Orthostatic hypotension testing is used to assess a patient's heart function, vasoconstriction, and hydration status, especially when they experience symptoms like syncope or blackouts.
- 😀 The test involves three positions: laying down, sitting up, and standing. Blood pressure is measured in each position to check for changes.
- 😀 The patient should be comfortable while laying down for a few minutes to allow their blood pressure to stabilize before measuring.
- 😀 The initial blood pressure reading while laying down should be normal, typically around 120/80 mmHg.
- 😀 After the patient sits up, blood pressure may drop slightly due to blood pooling in the legs and arms, which is expected.
- 😀 The blood pressure is measured quickly after the patient sits up, and any significant changes in the reading will be analyzed for potential issues.
- 😀 When standing, blood pools even further in the extremities, leading to a greater challenge for the body to maintain blood flow to the heart.
- 😀 If there is a large drop in blood pressure when moving from sitting to standing, it suggests a potential failure of compensatory mechanisms.
- 😀 Compensatory mechanisms include vasoconstriction (through alpha-1 receptors) and increased heart rate to maintain blood pressure.
- 😀 A significant drop in blood pressure (more than 20 mmHg systolic or 10 mmHg diastolic) or an increase in heart rate by more than 15 beats per minute indicates potential pathology, such as dehydration or poor vascular constriction.
Q & A
What is orthostatic hypotension testing used for?
-Orthostatic hypotension testing is used to assess a patient's heart function, vasoconstriction, and hydration status, particularly when they have symptoms like syncope or blacking out, which could be related to heart problems or dehydration.
What is the first step in conducting an orthostatic hypotension test?
-The first step is to have the patient lie down and remain in this position for a few minutes to ensure their blood pressure stabilizes before taking a baseline reading.
What is the significance of the baseline blood pressure measurement?
-The baseline blood pressure, typically around 120/80 mmHg, is important because it reflects the patient's normal blood pressure while lying down, serving as a reference for subsequent measurements.
Why is the blood pressure measured quickly after the patient sits up?
-Blood pressure is measured quickly after the patient sits up because the test is time-sensitive, and blood pressure may change rapidly as blood pools in the legs and arms upon sitting.
What changes are expected in blood pressure when the patient sits up from a lying down position?
-A slight drop in blood pressure is expected when the patient sits up, as blood pools in the legs and arms, causing reduced venous return to the heart. For example, the blood pressure might drop from 120/80 to around 118/78.
How does the body compensate when blood pressure drops after sitting up?
-The body compensates by increasing heart rate and causing vasoconstriction through Alpha 1 agonism, which helps to maintain blood pressure despite the reduced blood flow to the heart.
What is expected when the patient stands up during the orthostatic hypotension test?
-When the patient stands up, blood pressure is expected to drop further as blood pools more significantly in the legs and extremities. However, compensatory mechanisms should help stabilize the blood pressure.
What are the critical thresholds for diagnosing orthostatic hypotension?
-If the systolic blood pressure drops by 20 mmHg or more, or if the diastolic pressure drops by 10 mmHg or more, or if the heart rate increases by more than 15 beats per minute, it indicates potential orthostatic hypotension.
What could cause a failure of compensatory mechanisms during the test?
-A failure of compensatory mechanisms could be due to ineffective vasoconstriction, blood loss, or dehydration, which would result in insufficient blood volume or reduced vascular response to positional changes.
Why is the test done in three different positions (lying down, sitting, standing)?
-The test is done in three different positions to evaluate how the body responds to changes in posture and to assess the effectiveness of compensatory mechanisms in maintaining blood pressure and heart function in each position.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

How to Perform the Weber & Rinne Hearing Tests | Clinical Examination Skills

What is Spirometry? A patient Information Video

Exame de reticulócitos: para que serve e como é feito? Entenda de uma vez por todas!

Respiratory and Cardiac Aging Changes: Gerontology - Fundamentals of Nursing | @LevelUpRN

Pemeriksaan ABI (Ankle Brachial Index)
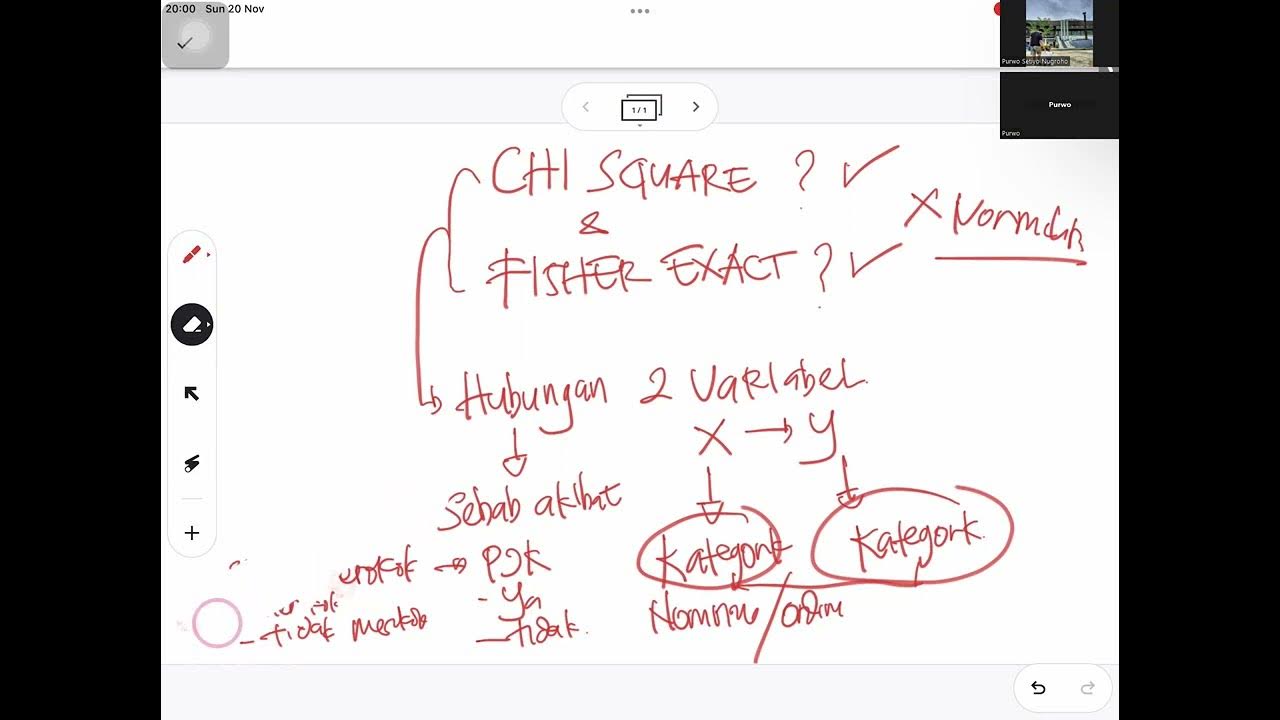
SYARAT MENGGUNAKAN UJI CHI SQUARE DAN FISHER EXACT
5.0 / 5 (0 votes)