IPE Core Competency Domain 1: Values/Ethics
Summary
TLDRThis video introduces the core competencies for interprofessional collaborative practice, focusing on the values and ethics competency. Using a patient scenario, it highlights how healthcare teams, including doctors, nurses, social workers, and pharmacists, work together to respect patient autonomy and provide compassionate, patient-centered care. The scenario involves Ella, a cancer patient transitioning to palliative care, and her daughter, Karen, who struggles to accept her mother's decision. The team demonstrates mutual respect, ethical decision-making, and collaboration in supporting Ella's wishes while managing the complexities of family dynamics in healthcare.
Takeaways
- 😀 Healthcare is evolving toward a collaborative, team-based approach to patient care, with a focus on teamwork competencies.
- 😀 Interprofessional education is crucial to prepare health professionals for working together in patient-centered care, as outlined in the Core Competencies for Interprofessional Collaborative Practice (2011).
- 😀 The first core competency, 'Values and Ethics for Interprofessional Practice,' emphasizes mutual respect and shared values among healthcare professionals when providing care.
- 😀 Confidentiality and respect for patient autonomy are key ethical considerations in team-based healthcare, especially in sensitive scenarios like palliative care decisions.
- 😀 The scenario illustrated a patient, Ella, who chose palliative care over further chemotherapy, which led to a need for sensitive team discussions and family involvement.
- 😀 Ella’s decision highlights the importance of respecting patient choices and supporting their dignity and privacy while collaborating with the healthcare team.
- 😀 The healthcare team’s role is to ensure patients like Ella can make informed decisions, with the support of trusted professionals from various disciplines, including oncologists, social workers, and pharmacists.
- 😀 Effective communication and mutual respect among team members and families are essential for addressing ethical dilemmas in healthcare, such as when a family member disagrees with a patient’s decision.
- 😀 The healthcare team is committed to providing ongoing support, pain management, and symptom control for Ella as she transitions to palliative care, while respecting her personal values and beliefs.
- 😀 A team-based approach to healthcare emphasizes the importance of understanding cultural diversity, individual patient needs, and fostering trust in relationships, both within the team and with patients and their families.
Q & A
What is the primary focus of interprofessional education in healthcare?
-The primary focus of interprofessional education is to prepare healthcare students to work together in teams, building competencies in collaboration to improve the quality, efficiency, and safety of patient care.
How does the Core Competencies for Interprofessional Collaborative Practice influence healthcare teams?
-The Core Competencies for Interprofessional Collaborative Practice, released in 2011, provide a framework for interprofessional education. They guide healthcare professionals to work collaboratively, ensuring that patient care is more efficient and comprehensive by utilizing the skills and expertise of different disciplines.
What does the first competency, 'values and ethics for interprofessional practice,' focus on?
-The first competency focuses on working from a base of shared values and mutual respect among healthcare professionals. It emphasizes the importance of delivering patient and population-centered care with ethical principles and recognizing the cultural diversity of patients and team members.
Why is confidentiality an important aspect of interprofessional collaborative practice?
-Confidentiality is crucial because it ensures that patient-practitioner relationships are respected within a team-based setting. Healthcare providers must maintain privacy while working collaboratively, ensuring that sensitive patient information is shared only with appropriate consent.
In the scenario, what decision did Ella make regarding her treatment plan?
-Ella decided, in collaboration with her healthcare team, to stop chemotherapy and transition to palliative care, focusing on symptom management and quality of life rather than further aggressive cancer treatments.
What is the role of the oncology social worker in this interprofessional team?
-The oncology social worker, Andrea, is responsible for providing psycho-social support to both the patient and family. In this case, she helps mediate the emotional aspects of Ella's decision and facilitates communication between Ella, her daughter Karen, and the healthcare team.
How does the healthcare team respect Ella’s autonomy in decision-making?
-The healthcare team respects Ella’s autonomy by honoring her decision to transition to palliative care. They ensure she is cognitively competent and fully informed about her choices, and they involve her in every step of the decision-making process, while also offering support to her family.
What was Karen’s reaction to her mother's decision, and how did the team address it?
-Karen, Ella's daughter, was initially unhappy with the decision, fearing her mother was giving up. The team acknowledged her concerns and suggested a family conference to address them, ensuring both Ella's wishes and Karen's emotional needs were respected.
How does the healthcare team handle ethical dilemmas in this case?
-The healthcare team handles ethical dilemmas by ensuring patient-centered care, maintaining confidentiality, and respecting both Ella’s wishes and her family’s concerns. They navigate difficult conversations with honesty and integrity while maintaining trust and mutual respect within the team.
What are some of the sub-competencies under the values and ethics competency for interprofessional practice?
-Sub-competencies include placing the interests of patients at the center of healthcare delivery, working in cooperation with those receiving care, embracing cultural diversity, and managing ethical dilemmas related to patient and population-centered care.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

What is interprofessional collaborative practice 1/7
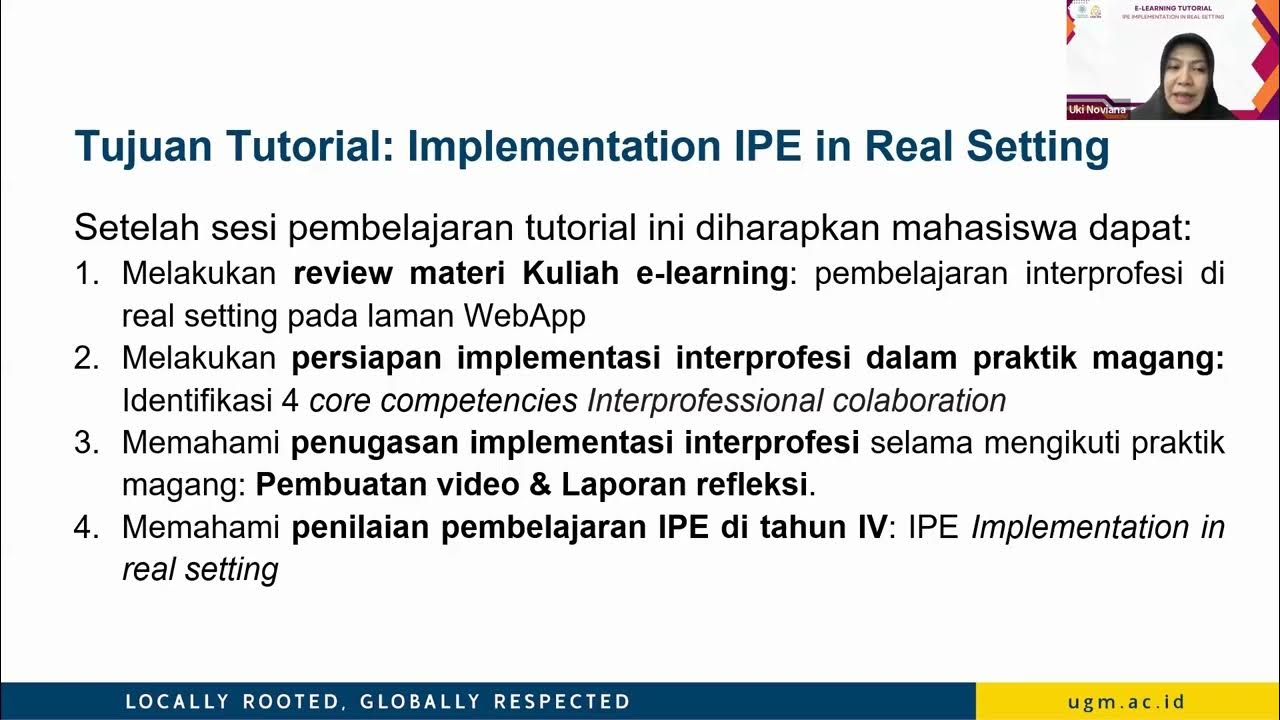
E-learning Tutorial Asinkron Semester 7

IPE Core Competency Domain 4: Teams and Teamwork

IPE Core Competency Domain 3: Interprofessional Communication

Introduction to interprofessional collaboration and interprofessional education

ICF Core Competency 4: Cultivates Trust and Safety
5.0 / 5 (0 votes)