Peritoneal Dialysis
Summary
TLDRThis video covers peritoneal dialysis, explaining its benefits compared to hemodialysis for patients with kidney dysfunction. It discusses key considerations like surgery requirements, patient independence, and suitability for those with unstable health conditions. The process involves using the peritoneum as a filtration membrane, with dialysate solution introduced via a catheter to filter waste, which is then drained. The video highlights the steps before, during, and after the procedure, patient education, and potential complications such as infections and hyperglycemia. It emphasizes proper care and technique to ensure patient safety and effectiveness.
Takeaways
- 🩺 Peritoneal dialysis is an alternative to hemodialysis, depending on the patient's condition, allowing faster access without needing months for a fistula to heal.
- ⏳ Patients who can't handle vascular access, anticoagulants, or have unstable conditions may benefit more from peritoneal dialysis compared to hemodialysis.
- 🏠 Peritoneal dialysis offers more independence as patients can perform the procedure at home without frequent trips to dialysis centers.
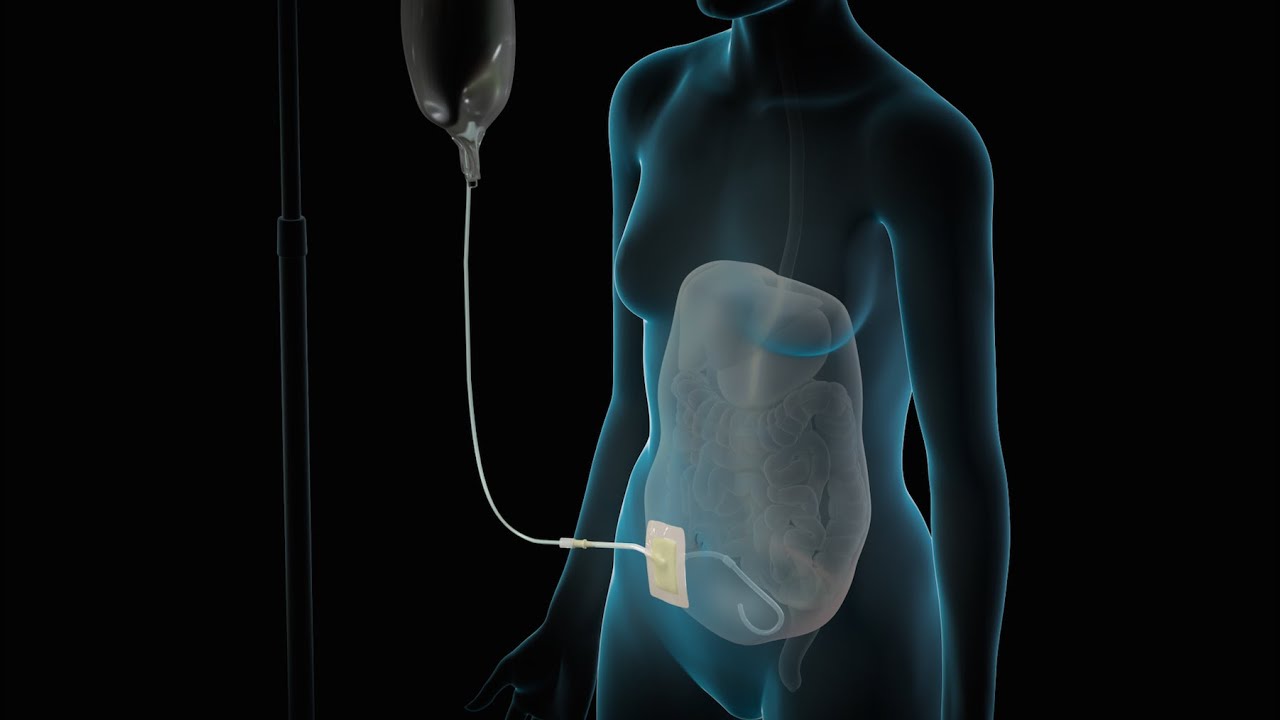
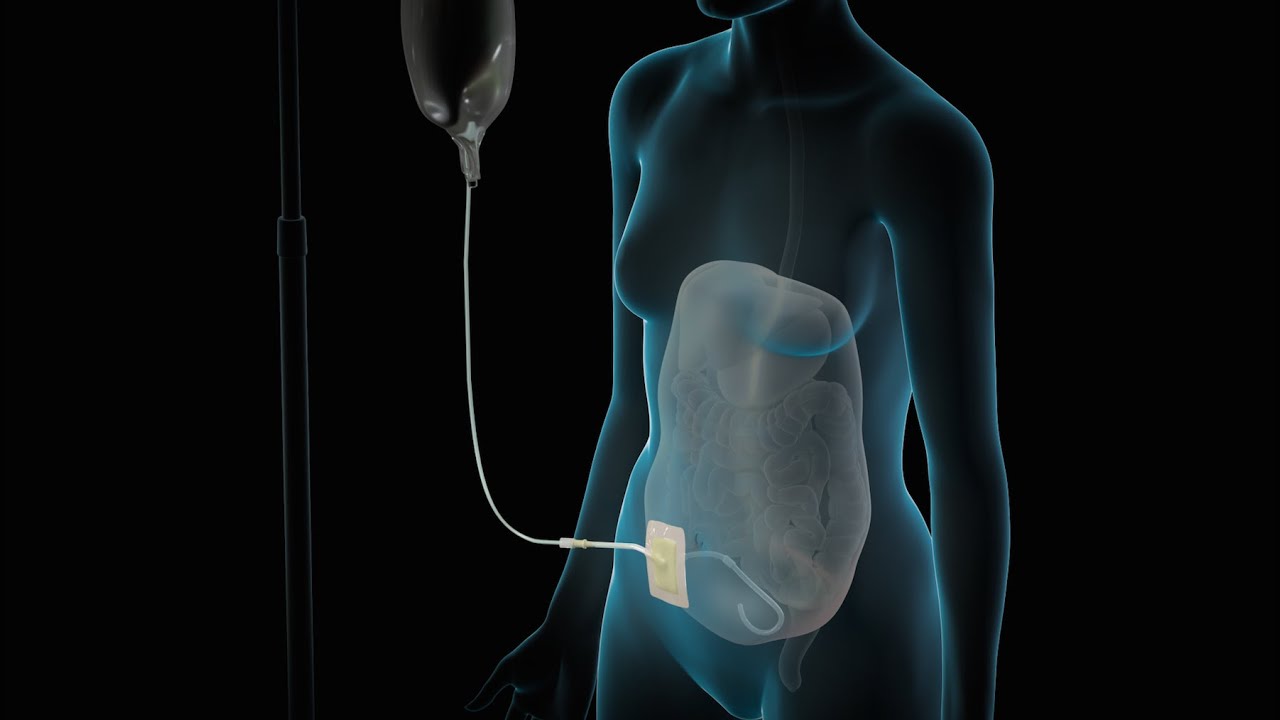
- 🧫 Peritoneal dialysis uses the peritoneum as a semi-permeable membrane to filter waste by instilling a sterile solution, which collects waste to be drained later.
- 🧪 Before starting peritoneal dialysis, a catheter is surgically placed for access, and patients undergo their first treatment in the hospital to ensure proper technique and monitoring.
- 📅 Two types of peritoneal dialysis exist: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD), with CAPD done multiple times daily and APD performed at night using a machine.
- 💧 Proper gravity-based setup is essential: the dialysate solution bag should be placed above shoulder height and the drainage bag below waist level to ensure effective waste removal.
- 🛑 Infection prevention is crucial, with careful monitoring of catheter sites for signs of redness, drainage, or discolored waste that could indicate infections or peritonitis.
- 🍬 Hyperglycemia can be a complication due to the hypertonic dialysate solution, so blood sugar monitoring is essential, especially in patients prone to high blood sugar.
- 🧼 Patient education focuses on proper catheter care, maintaining aseptic techniques, and recognizing signs of infection or complications to ensure successful home-based dialysis.
Q & A
What is the primary difference between peritoneal dialysis and hemodialysis in terms of surgery?
-Peritoneal dialysis allows for quicker use because a catheter can be placed and used without waiting. In contrast, hemodialysis requires a fistula or graft, which takes around six months to heal before it can be used.
Why might a patient opt for peritoneal dialysis over hemodialysis?
-A patient might choose peritoneal dialysis if they cannot handle the vascular access required for hemodialysis, if they have chronic infections or unstable hypertension, or if they want to maintain more independence by performing dialysis at home.
How does peritoneal dialysis work?
-Peritoneal dialysis uses the peritoneum, a semi-permeable membrane in the abdominal cavity, as a filtration system. A sterile solution is instilled into the cavity, which filters out waste, and then the waste is drained into a drainage bag.
What is 'dwell time' in peritoneal dialysis?
-'Dwell time' refers to the period when the dialysis solution sits in the abdominal cavity, allowing filtration to occur. After the dwell time, the waste is drained.
What are the two types of peritoneal dialysis mentioned in the video?
-The two types are Continuous Ambulatory Peritoneal Dialysis (CAPD), where dialysis occurs multiple times a day using gravity, and Automated Peritoneal Dialysis (APD), where a machine performs dialysis overnight.
What steps should a nurse take before a patient's first peritoneal dialysis session?
-The nurse should check the patient's weight, labs, and blood sugar levels, assess the catheter for proper function and cleanliness, and ensure the patient has signed consent forms.
What should be monitored during the peritoneal dialysis procedure?
-During the procedure, the nurse should monitor for any signs of infection at the catheter site, check the patient's vital signs, and ensure proper drainage and dwell times. The nurse should also educate the patient on proper technique and signs of complications.
What are common complications of peritoneal dialysis?
-Common complications include infections (especially at the catheter site), peritonitis (an infection of the abdominal lining), and hyperglycemia due to the hypertonic dialysis solution.
How can peritonitis be identified in a patient undergoing peritoneal dialysis?
-Peritonitis can be identified by cloudy or dark-colored drainage, fever, and abdominal pain, indicating an infection within the abdominal cavity.
What key points should be included in patient education for peritoneal dialysis?
-Patients should be educated on cleaning the catheter properly, maintaining sterile technique when connecting dialysis solutions, recognizing signs of infection, and monitoring their blood sugar levels for signs of hyperglycemia.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade Now5.0 / 5 (0 votes)