Kidney injuries 3
Summary
TLDRThis presentation discusses renal replacement therapies for kidney disease, covering various treatment methods such as hemodialysis, hemofiltration, peritoneal dialysis, and kidney transplantation. It explains how hemodialysis is the most common form of treatment, including its complications like hypertension and muscle cramps. Hemofiltration, which removes larger fluid volumes, and peritoneal dialysis, which allows patients to maintain mobility, are also explored. Finally, kidney transplantation is presented as the best long-term solution, though it comes with challenges like organ rejection and complications post-surgery. The session emphasizes the importance of effective management for successful outcomes.
Takeaways
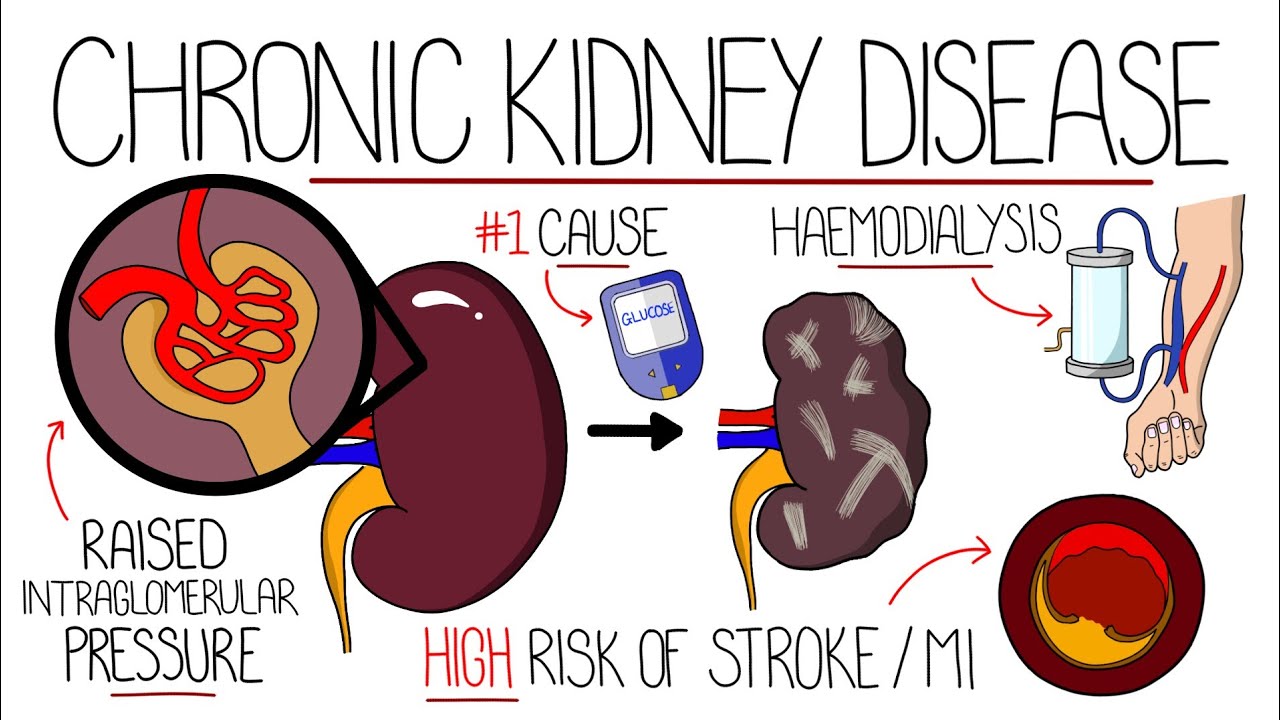
- 😀 Chronic kidney disease progression is measured by the glomerular filtration rate (GFR), with normal GFR ranging from 60 to 120 mL/min, and kidney failure GFR falling below 15 mL/min.
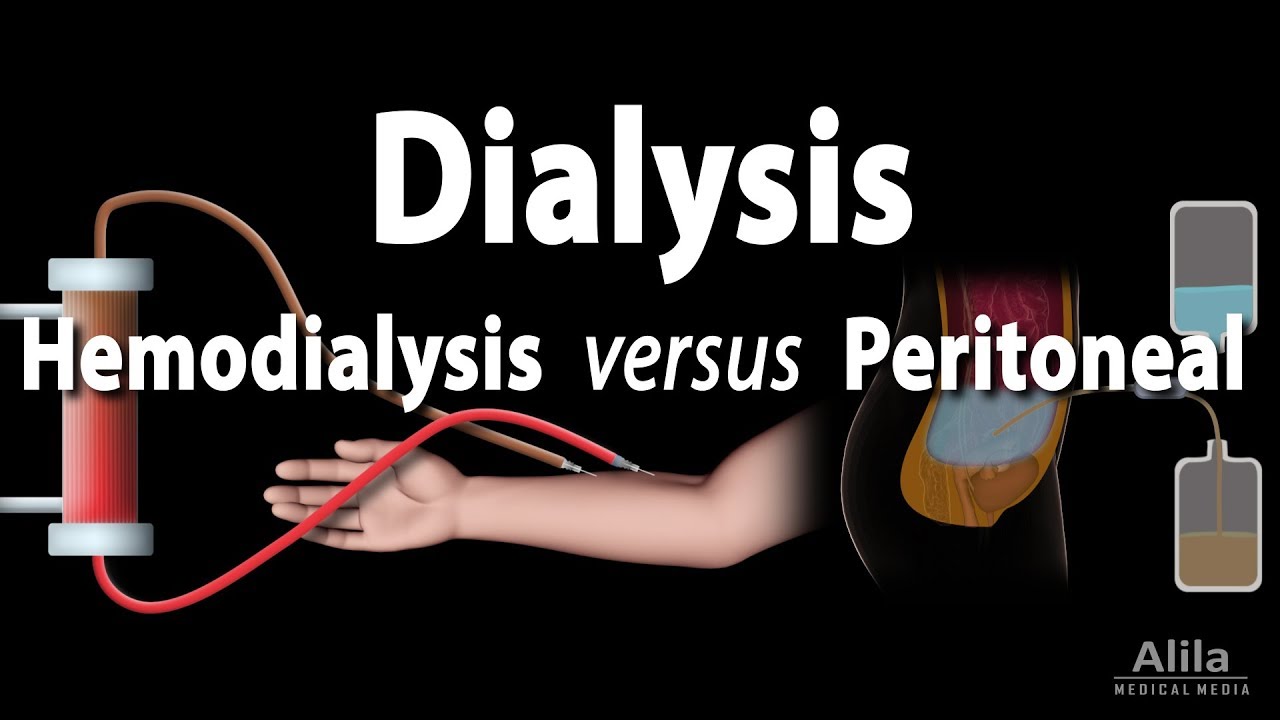
- 😀 Hemodialysis is the most common renal replacement therapy, used in both acute and chronic kidney injuries, where blood is filtered via a dialyzer with a semi-permeable membrane.
- 😀 Vascular access for hemodialysis is obtained via central venous catheter, or in the case of chronic kidney disease, an arteriovenous fistula is typically formed for repeated dialysis sessions.
- 😀 Common complications during hemodialysis include hypertension, muscle cramps, nausea, vomiting, headaches, chest pain, and itching, along with technical issues like clotting and air embolism.
- 😀 Hemofiltration is another renal replacement therapy, where large volumes of fluid are removed by ultrafiltration, differing from hemodialysis, which uses diffusion for solute movement.
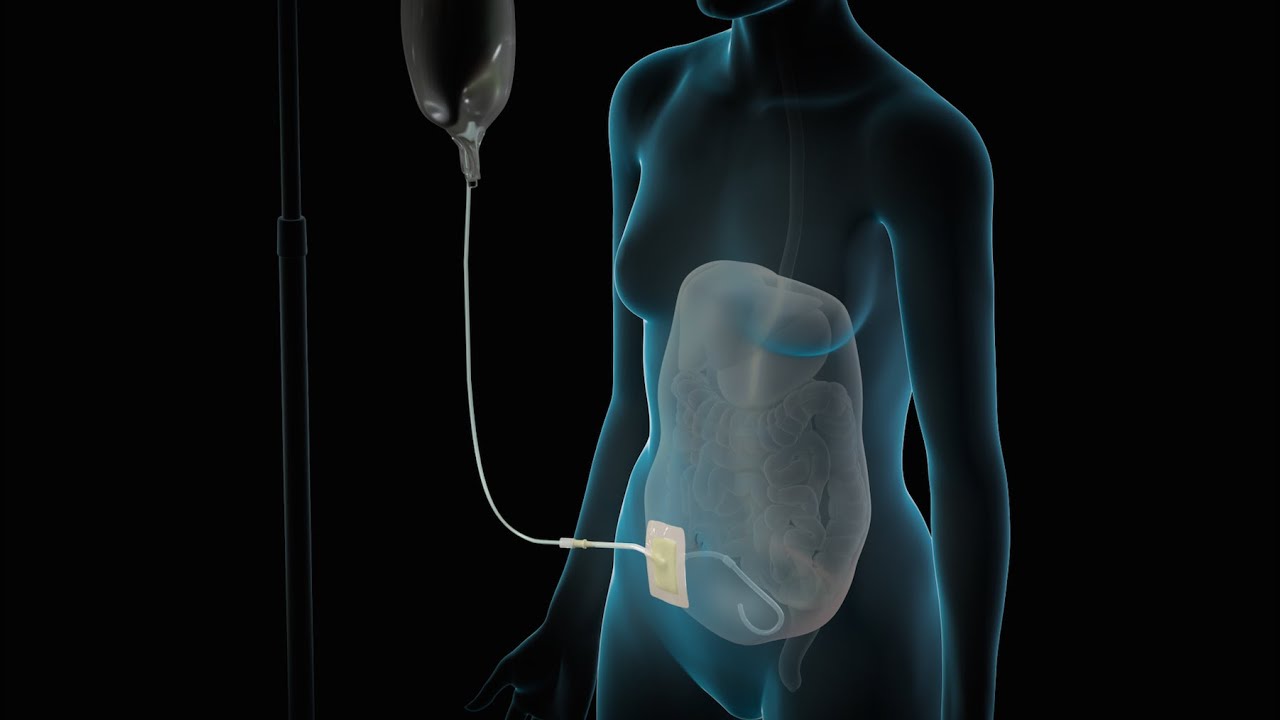
- 😀 Peritoneal dialysis uses the peritoneal membrane to remove waste products. It includes two types: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
- 😀 In CAPD, two liters of dialysis fluid are introduced into the peritoneal cavity for 4-6 hours, during which waste products diffuse into the fluid while the patient remains mobile.
- 😀 APD is similar to CAPD, but the fluid exchange is done with the aid of a mechanical device at night, allowing the patient to perform only a single exchange during the day.
- 😀 Kidney transplantation is the best long-term treatment for end-stage kidney disease and is the most cost-effective option, though matching a donor is challenging.
- 😀 Kidney transplant complications include bleeding, clotting, ureter blockages, organ rejection, infections, and cardiovascular issues, all of which must be managed effectively for transplant success.
Q & A
What does GFR stand for and what is its normal value?
-GFR stands for Glomerular Filtration Rate. The normal GFR is approximately 60 to 120 milliliters per minute.
What is the significance of GFR in kidney disease?
-The GFR helps assess kidney function. In kidney disease, GFR ranges from 15 to 60 milliliters per minute, and in kidney failure, GFR is less than 15 milliliters per minute.
What are the common renal replacement therapies used for kidney failure?
-The common renal replacement therapies include hemodialysis, hemofiltration, peritoneal dialysis, and renal transplantation.
How is hemodialysis performed in both acute and chronic kidney injury?
-In hemodialysis, blood is pumped through a dialyzer, where waste products are filtered across a semi-permeable membrane. In acute kidney injury, dialysis is performed through a large-bore catheter, while in chronic kidney injury, an arteriovenous fistula is commonly used.
What are some common complications that can occur during hemodialysis?
-Common complications during hemodialysis include hypertension, muscle cramps, nausea, vomiting, headaches, chest pain, and itching.
What is the difference between hemodialysis and hemofiltration?
-Hemodialysis involves the movement of small solutes by diffusion through a dialysis membrane, while hemofiltration removes larger volumes of fluid by ultrafiltration, resulting in the removal of solutes through convection.
What is peritoneal dialysis and how does it work?
-Peritoneal dialysis uses the peritoneal cavity as a filter. Dialysis fluid is introduced into the cavity, and waste products diffuse from the peritoneal capillaries into the fluid. It can be done in two forms: continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD).
What is the key difference between continuous ambulatory peritoneal dialysis and automated peritoneal dialysis?
-In continuous ambulatory peritoneal dialysis, the patient performs the dialysis exchanges manually, typically four times a day. In automated peritoneal dialysis, a machine performs the fluid exchange during the night, leaving the patient with only a single exchange to do during the day.
What are the potential complications associated with kidney transplantation?
-Kidney transplantation can lead to complications such as bleeding, clotting, ureter blockage, organ rejection, infections, cardiovascular diseases, and cancer spread.
Why is managing complications important after kidney transplantation?
-Managing complications is crucial for the success of the transplant and the long-term survival of the patient. Uncontrolled complications like infections or organ rejection can lead to transplant failure or other serious health issues.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video
Understanding Chronic Kidney Disease (CKD)

Polycystic Kidney Disease Explained

Kenali penyakit gagal ginjal kronis dan proses cuci darah

Peritoneal Dialysis: At Home Treatment for Kidney Failure | Mass General Brigham
Dialysis | Nucleus Health
Renal Replacement Therapy: Hemodialysis vs Peritoneal Dialysis, Animation
5.0 / 5 (0 votes)