The menstrual cycle
Summary
TLDRThe menstrual cycle is a 20-35 day process, averaging 28 days, that involves the ovaries and endometrium to facilitate reproduction. It encompasses the ovarian and uterine cycles, with ovulation typically at day 14. The cycle is regulated by hormones from the hypothalamus and pituitary gland, leading to the maturation of ovarian follicles and the thickening of the endometrium. After ovulation, the corpus luteum forms, secreting progesterone to prepare the endometrium for potential implantation. If fertilization doesn't occur, the cycle ends with menstruation, beginning a new cycle.
Takeaways
- 🔬 The menstrual cycle is a regular process involving the ovaries and endometrium that facilitates reproduction.
- 🌀 It consists of two synchronized processes: the ovarian cycle, focusing on follicle development and ovulation, and the uterine cycle, focusing on the endometrium's response to ovarian activity.
- 👧 Menarche marks the onset of the first menstrual period during early adolescence, and the cycle recurs monthly until menopause.
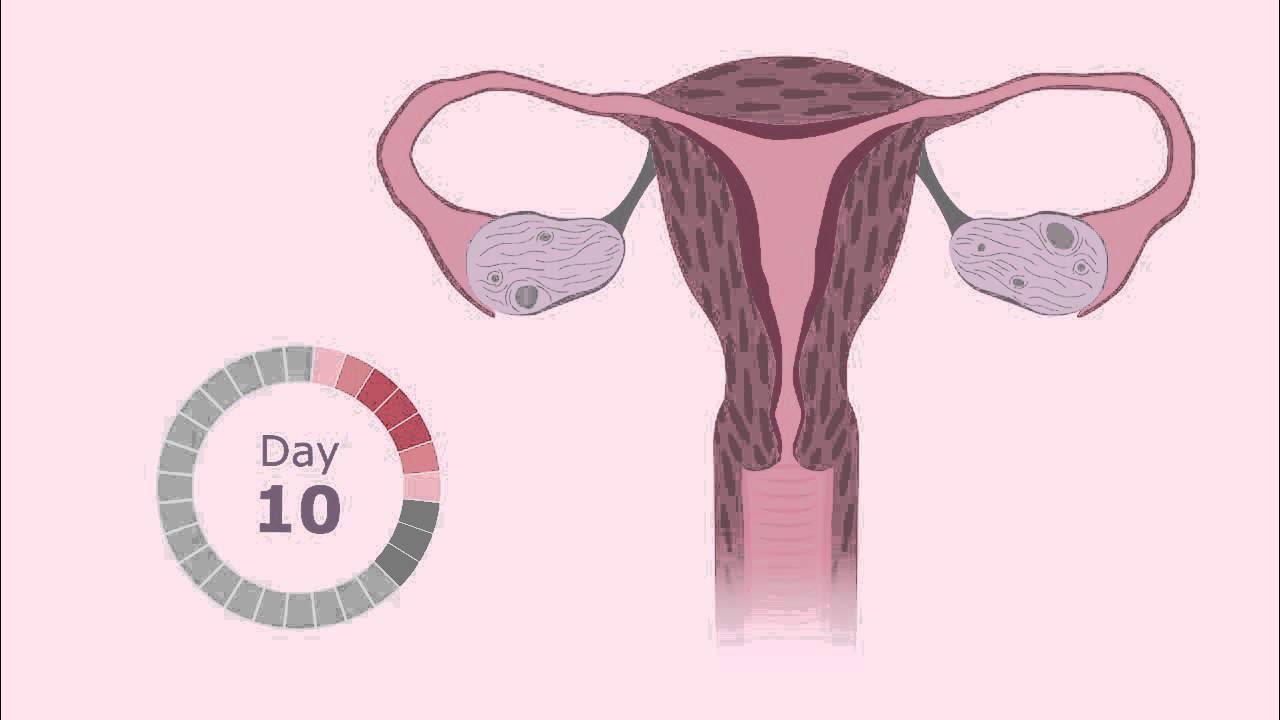
- ⏳ The menstrual cycle's length can vary from 20 to 35 days, averaging 28 days, with ovulation typically occurring 14 days before the start of menstruation.
- 📅 Each cycle begins on the first day of menstruation, with the preovulatory phase leading up to ovulation and the postovulatory phase following it.
- 🧠 The hypothalamus and pituitary gland control the menstrual cycle through the release of hormones like GnRH, FSH, and LH.
- 🌱 The ovarian follicular phase involves the maturation of ovarian follicles, with one becoming dominant and eventually undergoing ovulation.
- 🚀 A surge in FSH and LH, triggered by high estrogen levels, induces ovulation, releasing the oocyte from the dominant follicle.
- 🛡️ After ovulation, the ovarian follicle transforms into the corpus luteum, which secretes progesterone, becoming the dominant hormone of the luteal phase.
- 🌿 The endometrium undergoes the menstrual phase, proliferative phase, and secretory phase in response to hormonal changes throughout the cycle.
- 🌹 Progesterone prepares the endometrium for potential fertilization and implantation, and its decline signals the beginning of a new menstrual cycle.
Q & A
What is the menstrual cycle?
-The menstrual cycle refers to the regular changes in the ovaries and the endometrium that prepare the body for reproduction. It involves two interconnected processes: the ovarian cycle and the uterine or endometrial cycle.
What is the endometrium and what are its layers?
-The endometrium is the tissue lining the inside of the uterus, consisting of a functional layer that is shed during menstruation and a basal layer that supports the functional layer.
What are the two processes that make up the menstrual cycle?
-The two processes are the ovarian cycle, which involves the development of ovarian follicles and ovulation, and the uterine or endometrial cycle, which involves the thickening and shedding of the functional endometrium in response to ovarian activity.
What is menarche?
-Menarche is the onset of the first menstrual period, typically occurring during early adolescence as part of puberty.
How long does the average menstrual cycle last?
-The average menstrual cycle lasts about 28 days, but it can vary from 20 to 35 days.
When does ovulation typically occur in the menstrual cycle?
-Ovulation usually occurs 14 days before the first day of the next menstrual period, which is about day 14 of an average 28-day cycle.
What are the two phases of the menstrual cycle and what do they correspond to in the ovaries and endometrium?
-The two phases are the preovulatory phase, which includes the ovarian follicular phase and the endometrial proliferative phase, and the postovulatory phase, which includes the ovarian luteal phase and the endometrial secretory phase.
What role do the hypothalamus and pituitary gland play in the menstrual cycle?
-The hypothalamus and pituitary gland control the menstrual cycle by regulating the release of gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH), which in turn control the maturation of ovarian follicles and the endometrial changes.
What is the significance of the dominant follicle in the preovulatory phase?
-The dominant follicle is the one that continues to grow and eventually undergoes ovulation due to having the most follicle-stimulating hormone receptors, outcompeting other developing follicles.
What changes occur in the endometrium during the proliferative phase?
-During the proliferative phase, the endometrium thickens, endometrial glands grow, and spiral arteries emerge under the influence of estrogen, preparing the lining for potential implantation of a fertilized egg.
What happens after ovulation and how does it affect the endometrium?
-After ovulation, the remnants of the ovarian follicle form the corpus luteum, which secretes progesterone and estrogen, making the endometrium more receptive for implantation. This leads to the secretory phase of the endometrial cycle.
What is the role of progesterone during the luteal phase?
-Progesterone, secreted by the corpus luteum, acts as a negative feedback signal to the pituitary, decreasing the release of FSH and LH, and becomes the dominant hormone during the luteal phase, preparing the endometrium for potential implantation.
What triggers the beginning of a new menstrual cycle?
-The collapse of the spiral arteries and the shedding of the functional layer of the endometrium, which occurs when progesterone levels decrease, triggers menstruation and the beginning of a new menstrual cycle.
Outlines

Этот раздел доступен только подписчикам платных тарифов. Пожалуйста, перейдите на платный тариф для доступа.
Перейти на платный тарифMindmap

Этот раздел доступен только подписчикам платных тарифов. Пожалуйста, перейдите на платный тариф для доступа.
Перейти на платный тарифKeywords

Этот раздел доступен только подписчикам платных тарифов. Пожалуйста, перейдите на платный тариф для доступа.
Перейти на платный тарифHighlights

Этот раздел доступен только подписчикам платных тарифов. Пожалуйста, перейдите на платный тариф для доступа.
Перейти на платный тарифTranscripts

Этот раздел доступен только подписчикам платных тарифов. Пожалуйста, перейдите на платный тариф для доступа.
Перейти на платный тарифПосмотреть больше похожих видео

Ciclo Menstrual (menstruação) e Ovulação - Sistema Reprodutor Feminino - VideoAula 050

Fisiologi Siklus Menstruasi (5/5) - Siklus Menstruasi Normal
The Menstrual Cycle

ovulation and menstrual cycle often called period|medical animationDandelionTeam #ovulation #period

Ciclo menstrual - Biologia - Ensino Médio

Alat Reproduktif Wanita
5.0 / 5 (0 votes)
