Understanding Jugular Venous Pressure (JVP)
Summary
TLDRIn this video, Tom from Zero to Finals explains how to assess the Jugular Venous Pressure (JVP), an indirect measure of right atrium pressure. He walks through the complexities of JVP measurement, focusing on the visualization of the right internal jugular vein and the identification of its characteristic waveform. Tom breaks down the JVP's five phases—A wave, X descent, C wave, V wave, and Y descent—while clarifying the physiological events behind each. He also highlights how to identify common abnormalities, such as large A or V waves, and offers practical advice for practicing JVP assessment. The video is a helpful resource for those studying cardiovascular health.
Takeaways
- 😀 The jugular venous pressure (JVP) is a measure of pressure in the right atrium and venous system, with higher pressure indicating higher JVP.
- 😀 JVP assessment is done by observing the right internal jugular vein, as it is closest to the right atrium, giving the best indication of atrial pressure.
- 😀 To visualize the JVP, the patient should sit at a 45-degree angle and turn their head slightly to the left, with light shining diagonally across the neck.
- 😀 The JVP pulsation is characterized by two pulses for each heartbeat, which is different from the carotid pulse, which only has one pulse per beat.
- 😀 A JVP pulsation can’t be palpated, unlike the carotid pulse, which can be felt with your fingers.
- 😀 The hepatojugular reflex is used to confirm JVP by pressing on the liver, temporarily raising the JVP.
- 😀 Normal JVP height is less than 3 cm, and a height above 3 cm is considered a raised JVP, indicating potential health issues.
- 😀 The JVP waveform consists of five phases: the A wave, X descent, C wave, the second part of the X descent, the V wave, and the Y descent.
- 😀 The A wave occurs during atrial contraction, raising the JVP as blood is pushed into the right ventricle and up into the jugular vein.
- 😀 The C wave is caused by the tricuspid valve bulging into the atrium during ventricular contraction, which increases pressure in the JVP.
- 😀 Abnormalities in JVP, such as absent A waves (in atrial fibrillation), large A waves (right ventricular hypertrophy or tricuspid stenosis), and large V waves (tricuspid regurgitation), can indicate specific cardiac conditions.
Q & A
What is jugular venous pressure (JVP) and why is it important?
-JVP is an indirect measurement of the pressure in the right atrium and venous system. It is important because changes in JVP can help identify conditions like heart failure, fluid overload, constrictive pericarditis, and cardiac tamponade.
Why do we assess the right internal jugular vein (IJV) for JVP?
-The right internal jugular vein is assessed because it is most directly aligned with the right atrium, providing the most accurate reflection of the pressure in the right atrium.
How do you position a patient to assess JVP effectively?
-The patient should be seated at a 45-degree angle with their head slightly turned to the left. This position allows optimal visualization of the right internal jugular vein and its pulsations.
What is the normal height for JVP, and what does a height above 3 cm indicate?
-The normal height of JVP is less than 3 cm. A height above 3 cm is considered elevated, which may indicate an underlying condition such as heart failure or fluid overload.
How can you differentiate between JVP and carotid pulse during examination?
-The JVP has two pulsations per heart beat, while the carotid pulse has only one. Additionally, JVP cannot be palpated, whereas the carotid pulse can be felt.
What is the hepatojugular reflex and how is it related to JVP assessment?
-The hepatojugular reflex is when pressure is applied to the liver or right upper abdomen, causing a temporary rise in JVP. It helps confirm the presence of an elevated JVP.
Can you describe the five components of the JVP waveform?
-The five components of the JVP waveform are: 1) A wave (atrial contraction), 2) X descent (atrial relaxation and blood flow into the ventricle), 3) C wave (right ventricular contraction and tricuspid valve bulging), 4) V wave (right atrial filling), and 5) Y descent (emptying of the right atrium into the ventricle).
What causes the C wave in the JVP waveform?
-The C wave is caused by the bulging of the tricuspid valve into the right atrium during right ventricular contraction, which increases pressure in the internal jugular vein.
How can you identify abnormalities in the JVP waveform?
-Abnormalities in JVP can include absent A waves (in atrial fibrillation), large A waves (due to right ventricular hypertrophy or tricuspid stenosis), and large V waves (caused by tricuspid regurgitation).
What is the significance of large V waves in the JVP waveform?
-Large V waves indicate tricuspid regurgitation, where blood flows backward into the right atrium, causing increased pressure and prominent filling of the superior vena cava and internal jugular vein.
Outlines

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantMindmap

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantKeywords

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantHighlights

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantTranscripts

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantVoir Plus de Vidéos Connexes

Prosedur Keperawatan - Pengukuran Central Venous Pressure (CVP)

CSL FK - Pemeriksaan Tekanan Vena Jugularis atau Jugular Venous Pressure (JVP)

Pengukuran dan Perawatan Central Venous Pressure (CVP)

Mechanisms of Venous Return, Animation

Pemeriksaan Fisik Sistem Kardiovaskular
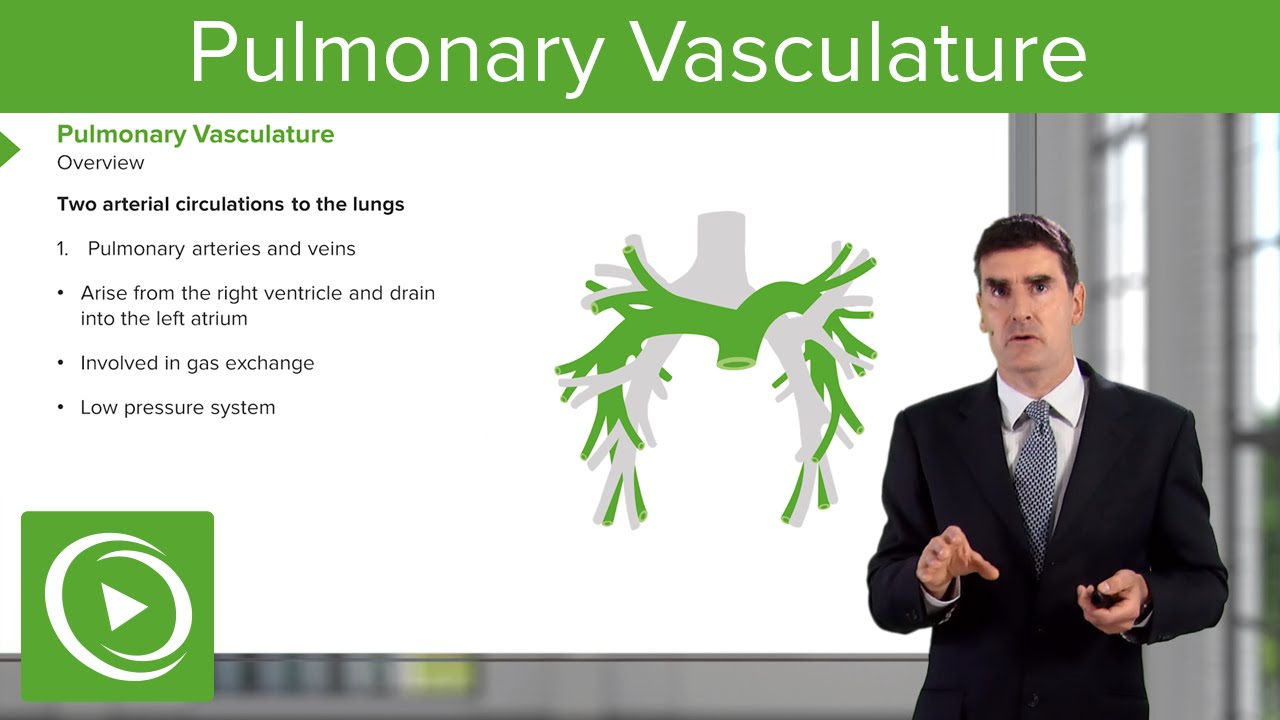
Pulmonary Vasculature – Respiratory Medicine | Medical Education Videos
5.0 / 5 (0 votes)
