Pengukuran dan Perawatan Central Venous Pressure (CVP)
Summary
TLDRThis video script provides an in-depth explanation and demonstration of Central Venous Pressure (CVP) measurement and care. It outlines the procedure for inserting a catheter into central veins to measure pressure within the superior vena cava, reflecting the right atrium's pressure and heart function. The script also covers important factors such as patient positioning, types of equipment used, and the interpretation of CVP values to assess fluid balance. The video includes practical steps for measuring and maintaining the catheter site, emphasizing patient care and sterile techniques to avoid infection.
Takeaways
- 😀 Central venous pressure (CVP) is the measurement of pressure in the central veins, reflecting right atrium pressure and indirectly indicating the preload of the right heart.
- 😀 The measurement of CVP is affected by intrathoracic pressure, which fluctuates with respiration, especially in patients with respiratory issues.
- 😀 CVP values typically range between 3-10 cm H2O or 3-10 mmHg, with variations based on different sources and patient conditions.
- 😀 In patients with asthma or COPD, CVP should be measured during inhalation to avoid inaccurate readings due to airway obstruction.
- 😀 An increase in CVP often indicates fluid overload, whereas a decrease suggests dehydration or insufficient fluid volume.
- 😀 Common causes of elevated CVP include right heart failure, cardiac tamponade, pulmonary hypertension, or mechanical ventilation.
- 😀 Decreased CVP can be caused by vasodilation, increased intrathoracic pressure, or dysfunction of the sympathetic nervous system.
- 😀 The installation of a CVP catheter is essential for managing fluid balance, guiding fluid replacement therapy, and assessing circulatory failure in critical patients.
- 😀 The procedure to insert a CVP catheter requires careful preparation, including obtaining patient consent, ensuring sterilization, and selecting the appropriate catheter type.
- 😀 Proper positioning of the patient and careful measurement of zero points are critical steps in accurate CVP measurement, especially when using a manometer.
- 😀 After CVP measurement, sterile techniques must be followed during catheter care and dressing changes to avoid infection and ensure proper catheter function.
Q & A
What is the purpose of Central Venous Pressure (CVP) measurement?
-The purpose of CVP measurement is to assess the pressure in the central venous system, which reflects the pressure in the right atrium and indirectly in the right ventricle, aiding in the evaluation of fluid balance, heart function, and circulatory health.
What are the normal values for CVP?
-Normal CVP values typically range from 3-10 cm H2O or 2-6 mmHg, though variations might exist depending on specific medical sources.
How is CVP measured?
-CVP is measured by inserting a flexible catheter into a central vein, such as the subclavian or jugular vein, and using a manometer or transducer to monitor the pressure within the catheter, which reflects the central venous pressure.
Why should CVP measurement be done at the end of expiration?
-CVP measurements should be taken at the end of expiration to avoid respiratory influences on intrathoracic pressure, ensuring the measurement is stable and more accurate.
What might a high CVP indicate?
-A high CVP indicates fluid overload and may suggest conditions such as right heart failure, pulmonary hypertension, or tamponade.
What might a low CVP indicate?
-A low CVP suggests that the patient is dehydrated or experiencing low blood volume, which could be due to hemorrhage or severe fluid loss.
What are the common complications that can affect CVP measurement?
-Common complications include incorrect catheter placement, obstruction or displacement of the catheter, inaccurate zeroing of the measurement system, or equipment malfunction. Respiratory variations, such as changes during mechanical ventilation, can also affect readings.
Why is patient positioning important during CVP measurement?
-Proper patient positioning, typically in a supine position with the head slightly lowered, ensures accurate measurement by aligning the catheter correctly with the heart and central venous system for optimal pressure readings.
What are the typical indications for inserting a CVP catheter?
-CVP catheter insertion is indicated for monitoring fluid balance, guiding fluid therapy in conditions like shock or heart failure, evaluating the effects of medications, and assisting in procedures like dialysis or hemofiltration.
What steps are involved in the maintenance and care of a CVP catheter insertion site?
-Care for the CVP insertion site includes checking for signs of infection, ensuring the catheter remains in place, changing dressings using sterile techniques, and performing regular monitoring to ensure the catheter functions correctly without blockages.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Prosedur Keperawatan - Pengukuran Central Venous Pressure (CVP)

🔴 MONITORIZAÇÃO HEMODINÂMICA EXPLICADA 🔴

Monitorização Hemodinâmica

Blood Gas Interpretation Made Easy (Learn How To Interpret Blood Gases In 11 Minutes)

Primäre Hämostase - Teil 2 - Physiologie und Medikamente - AMBOSS Auditor
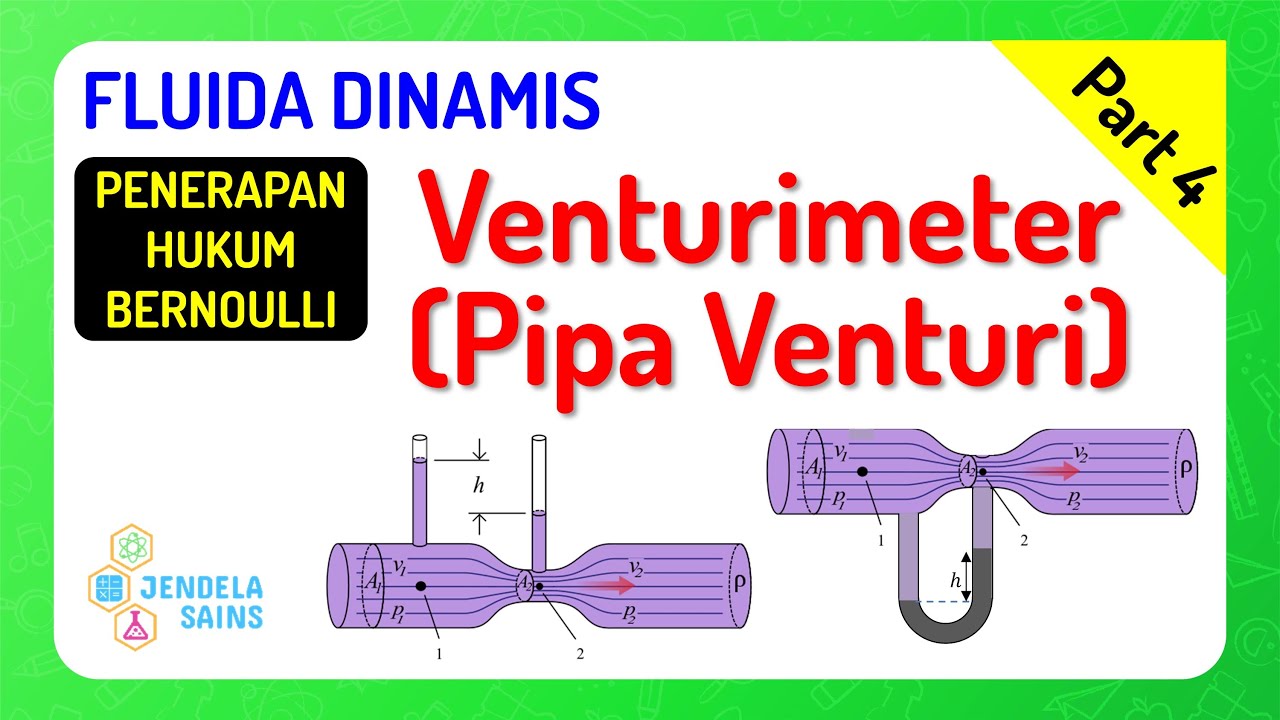
Fluida Dinamis • Part 4: Venturimeter / Pipa Venturi
5.0 / 5 (0 votes)