QSEN: The Lewis Blackman Story (Part Three)
Summary
TLDRThe transcript discusses the need for a patient-centered culture in healthcare, emphasizing the importance of communication and respect. The speaker recounts an experience where a lack of responsiveness from medical staff created barriers to care. They highlight the need for empowered nurses and physicians to listen and engage with patients, suggesting that better teamwork and understanding could prevent similar situations. The speaker also points out the absence of visible teamwork and the challenges faced when trying to navigate the healthcare system during a crisis.
Takeaways
- 🔑 Empowerment through communication: The patient's family felt empowered if a nurse had listened and engaged in a collaborative discussion to address their concerns.
- 🚫 Lack of responsiveness: The family faced a lack of responsiveness from the medical staff, which included both nurses and physicians.
- 🗣️ Importance of clear communication: The family emphasized the importance of being heard and understood, especially when they were advocating for their son's health.
- 👨⚕️ Role of the attending physician: The attending physician was seen as a roadblock due to their unavailability and unwillingness to be contacted.
- 🏥 Hospital environment impact: The family felt that the hospital's quiet Sunday afternoon setting contributed to the lack of immediate action.
- 📞 Lack of knowledge about hospital procedures: The family was unaware of how to contact the necessary medical staff or even the existence of a supervisor for the nurse.
- 👥 Absence of teamwork: The script suggests that there was no visible teamwork among the nursing or medical staff, which could have improved the situation.
- 🤔 Need for moral accountability: There was a perceived lack of moral accountability among the healthcare providers, who did not acknowledge their roles in the patient's care.
- 👶 Vulnerability of different patients: The family recognized that their situation could be worse for patients who lack communication skills or have more severe conditions.
- 📢 Advocacy for change: The script implies a need for systemic changes to foster a more patient-centered culture within healthcare institutions.
Q & A
What was the main issue the speaker faced with the healthcare system?
-The main issue was a lack of a patient-centered culture, where the speaker felt helpless due to roadblocks in communication with healthcare providers and a lack of responsiveness to their concerns.
What specific actions could have made the speaker feel more empowered?
-The speaker would have felt more empowered if there was a nurse who listened to them and engaged in a give-and-take discussion to lay out a plan of action, including calling the attending physician.
Why did the speaker feel that their communication was not taken seriously?
-The speaker felt that their communication was not taken seriously because the healthcare providers did not believe them and did not understand the seriousness of the situation, despite the speaker's son being articulate and having no communication issues.
What was the situation like for the speaker on that Sunday afternoon?
-On that Sunday afternoon, the hospital was nearly empty, with only an intern and a nurse present, who did not believe or understand the seriousness of the speaker's situation.
What did the speaker not know about the hospital's procedures?
-The speaker did not know about the existence of a supervisor for the nurse, how to contact the doctors outside of the hospital, or that the doctors might have an answering service.
What is the role of the administrator on-call in this context?
-The administrator on-call is expected to have a significant influence on ensuring things go well within the hospital, and they should be aware of who the on-call person is at any given time.
What did the speaker observe about the moral accountability of the individuals involved?
-The speaker observed a lack of moral accountability, as there was no acknowledgment of the healthcare providers' responsibilities in addressing the speaker's concerns.
How did the speaker perceive the teamwork within the healthcare setting?
-The speaker did not observe any teamwork, as there was no evidence of coordinated effort or communication among the nursing, medical, or overall healthcare team.
What was the speaker's experience with the Rapid Response Teams?
-The speaker mentioned Rapid Response Teams as a potential solution to the problem of healthcare providers not wanting to be bothered, but did not provide specific details about their experience with these teams.
What is the speaker's suggestion for teaching people not to be intimidated in healthcare settings?
-The speaker suggests that there are specialists who can teach people not to be intimidated, though they do not provide specifics on how this is done.
What information should South Carolina hospitals provide to patients according to the speaker?
-South Carolina hospitals are required to provide certain information about emergency numbers to patients, but the speaker implies that the information may not be clear or easily interpretable as emergency contact information.
Outlines

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantMindmap

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantKeywords

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantHighlights

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantTranscripts

Cette section est réservée aux utilisateurs payants. Améliorez votre compte pour accéder à cette section.
Améliorer maintenantVoir Plus de Vidéos Connexes

IPE Core Competency Domain 3: Interprofessional Communication

Patient- and Family-Centered Care - The University of Vermont Medical Center
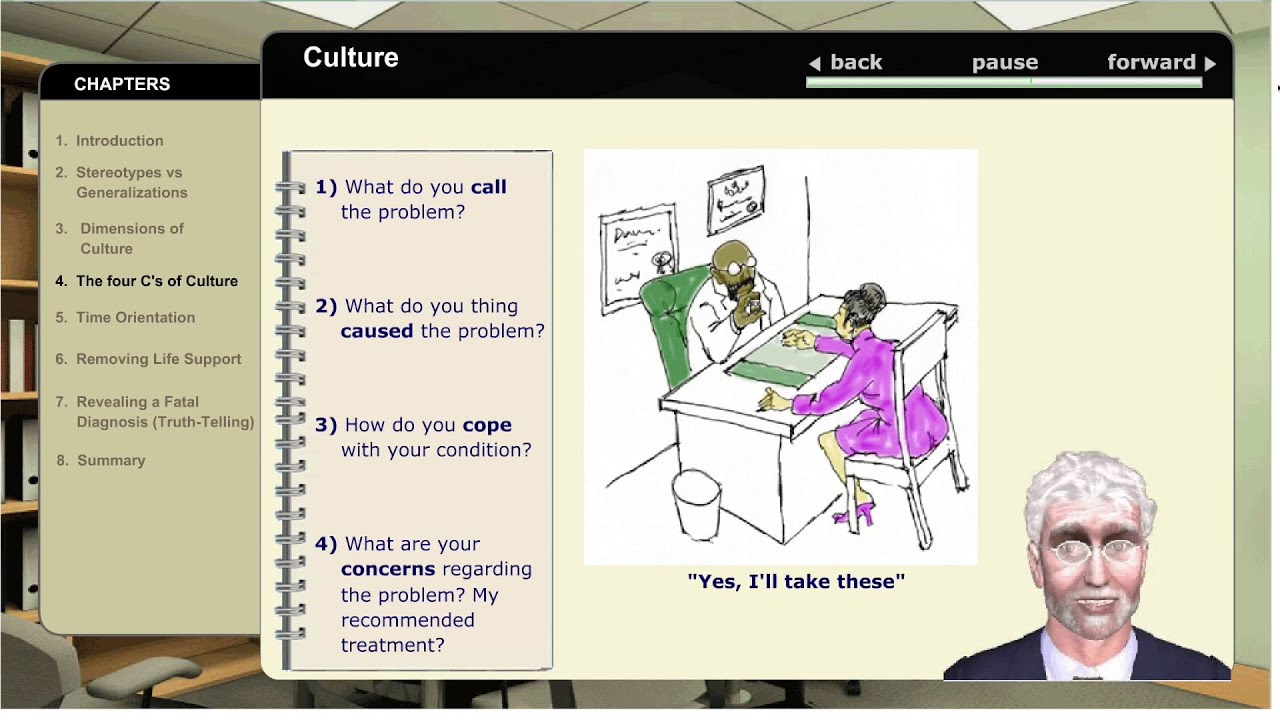
The 4C's - Understanding Cultural Diversity In Healthcare

Why does interprofessional collaboration matter The Triple Aim in Healthcare 3/7

Caso N°2 - Modulo II

Professionalism and Code of Conduct lect 7
5.0 / 5 (0 votes)
