FUNGAL ACNE "SAFE" SKINCARE EXPLAINED | Dermatologist
Summary
TLDRThis video script delves into the misconceptions surrounding 'fungal acne,' which is actually a condition known as pitted keratolysis or malassezia folliculitis. Caused by the yeast malassezia, it thrives in oily, moist environments and can affect those with weakened immune systems or those using topical steroids. The script clarifies that skincare products don't cause this yeast overgrowth and emphasizes the importance of seeing a dermatologist for proper diagnosis and treatment. It also discusses various treatments, including topical and oral anti-fungal medications, and lifestyle changes to manage and prevent recurrences, debunking the myth of 'fungal acne safe' skincare products.
Takeaways
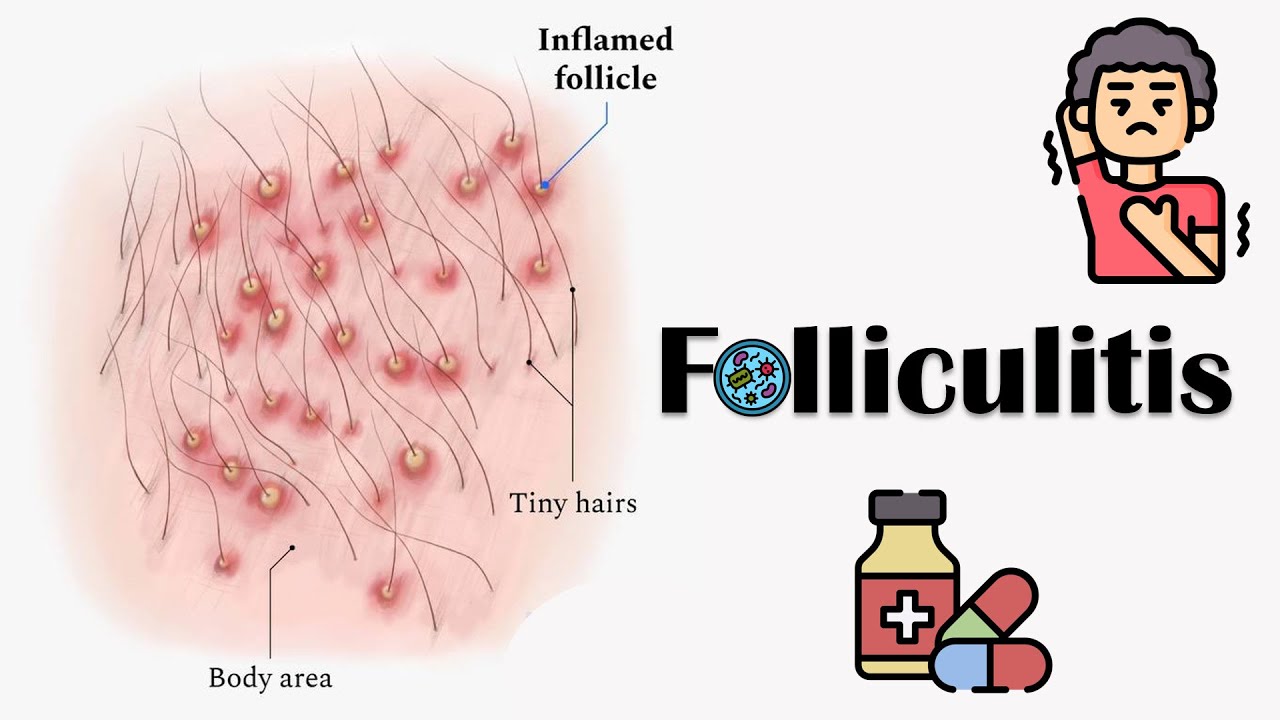
- 🔍 Fungal acne is a misnomer; the correct term is Pityrosporum folliculitis or Malassezia folliculitis, which is a type of folliculitis, not acne.
- 🌱 Malassezia is a yeast that naturally lives on the skin and can cause various skin conditions like dandruff, seborrheic dermatitis, and tinea versicolor.
- 💡 Malassezia folliculitis is more common in people with weakened immune systems, such as those with HIV, or those taking medications that suppress the immune system.
- 🌡 The yeast thrives in hot, moist, and humid environments, making it prevalent in tropical settings and among people who wear tight clothing or have hyperhidrosis.
- 🚫 Prolonged use of oral antibiotics can disrupt skin microflora, potentially leading to an overgrowth of Malassezia.
- 🔍 Malassezia folliculitis presents as red bumps and pustules around hair follicles, differing from acne by lacking blackheads and whiteheads.
- 🚫 There is no such thing as 'fungal acne safe' skincare products, as products do not feed Malassezia, which is sustained by sebum, not ingredients in skincare.
- 🧴 Skincare products can help remove excess oil from the skin's surface but do not directly influence sebum production.
- 🌡 Heavy or occlusive products can exacerbate the condition by slowing down sweat evaporation, leading to increased sweating and a favorable environment for Malassezia.
- 💊 Treatment for Malassezia folliculitis typically starts with topical anti-fungal agents, such as anti-dandruff shampoos or Nizoral shampoo with ketoconazole.
- 👕 Lifestyle changes like wearing lightweight, breathable clothing and avoiding occlusive fabrics can help manage and prevent recurrences of the condition.
Q & A
What is the correct medical term for what is commonly referred to as 'fungal acne'?
-The correct medical term is either pitted keratolysis or malassezia folliculitis, not acne.
What is the role of the malassezia yeast in skin conditions?
-Malassezia is a yeast that naturally lives on everyone's skin and can cause different skin conditions such as dandruff, seborrheic dermatitis, tinea versicolor, and head and neck dermatitis under certain circumstances.
Why is the condition called malassezia folliculitis not actually acne?
-Malassezia folliculitis is a type of folliculitis, which is an inflammation around the hair follicle, whereas acne is a problem with clogged pores and is not caused by the malassezia yeast.
Which populations are more commonly affected by malassezia folliculitis?
-People with weakened immune systems, such as patients in hospitals, those with HIV, or those taking medications that weaken the immune system, are more commonly affected.
What environmental factors contribute to the development of malassezia folliculitis?
-Hot, moist, and humid environments, as well as wearing tight or occlusive clothing that traps moisture, can contribute to the development of malassezia folliculitis.
How does the use of oral antibiotics relate to the development of malassezia folliculitis?
-Oral antibiotics can disrupt the skin microflora, potentially leading to an overgrowth of malassezia within the hair follicle, which may result in malassezia folliculitis.
What are some distinguishing features of malassezia folliculitis compared to acne?
-Malassezia folliculitis presents as monomorphic red bumps and pus bumps that overlay a hair follicle, are itchy, and do not have blackheads or whiteheads, unlike acne.
Can a person have both acne and malassezia folliculitis simultaneously?
-Yes, it is possible to have both conditions at the same time, especially since acne treatments may involve oral antibiotics which could lead to the development of malassezia folliculitis.
What is the general advice for treating malassezia folliculitis?
-The first line of treatment typically involves topical anti-fungal agents, and it's important to see a dermatologist for an accurate diagnosis and treatment plan.
What is the role of isotretinoin in treating malassezia folliculitis?
-Isotretinoin, also known as Accutane, is a treatment option for those with frequent recurrences of malassezia folliculitis, as it is the only therapy that shrinks the oil glands and suppresses sebum production.
What is the significance of photodynamic therapy in treating malassezia folliculitis?
-Photodynamic therapy can help destroy malassezia spores and is anti-inflammatory, potentially providing a recurrence-free period for some individuals with malassezia folliculitis.
Outlines

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraMindmap

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraKeywords

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraHighlights

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraTranscripts

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraVer Más Videos Relacionados

Keseringan Cuci Muka Bisa Bikin Jerawat? | SeKiLas

Micologia, Virologia e Microbiologia Clínica 01/02
Folliculitis - Causes, Signs & Symptoms, Complications & Treatment

Episodio #309 Tinnitus, zumbido en los Oídos

Signs of over-moisturizing the skin // Can you MOISTURIZE TOO MUCH? @DrDrayzday

Integumentary System Part 3 (Part 3 Of 3) (Skin Diseases)
5.0 / 5 (0 votes)
