Neuro Short Case Made Easy 1 (Proximal Weakness) - by Prof. Dr. Lim Kheng Seang
Summary
TLDRThis transcript delves into the examination of neurological cases, focusing on limb examinations and differential diagnoses for upper and lower motor neuron lesions. The discussion highlights how to interpret findings like proximal or distal weakness, reflex changes, and tone abnormalities to identify conditions such as polyneuropathy, myopathy, and spinal cord lesions. The speaker emphasizes the importance of localized signs, using a structured approach to narrow down diagnoses, and provides specific examples, including conditions like CIDP, cervical myelopathy, and polymyositis. It stresses the need for thorough examination and clinical reasoning to pinpoint the correct pathology.
Takeaways
- 😀 Neurological examinations focus on differentiating between upper motor neuron (UMN) and lower motor neuron (LMN) lesions, which require careful observation of signs like tone, power, and reflexes.
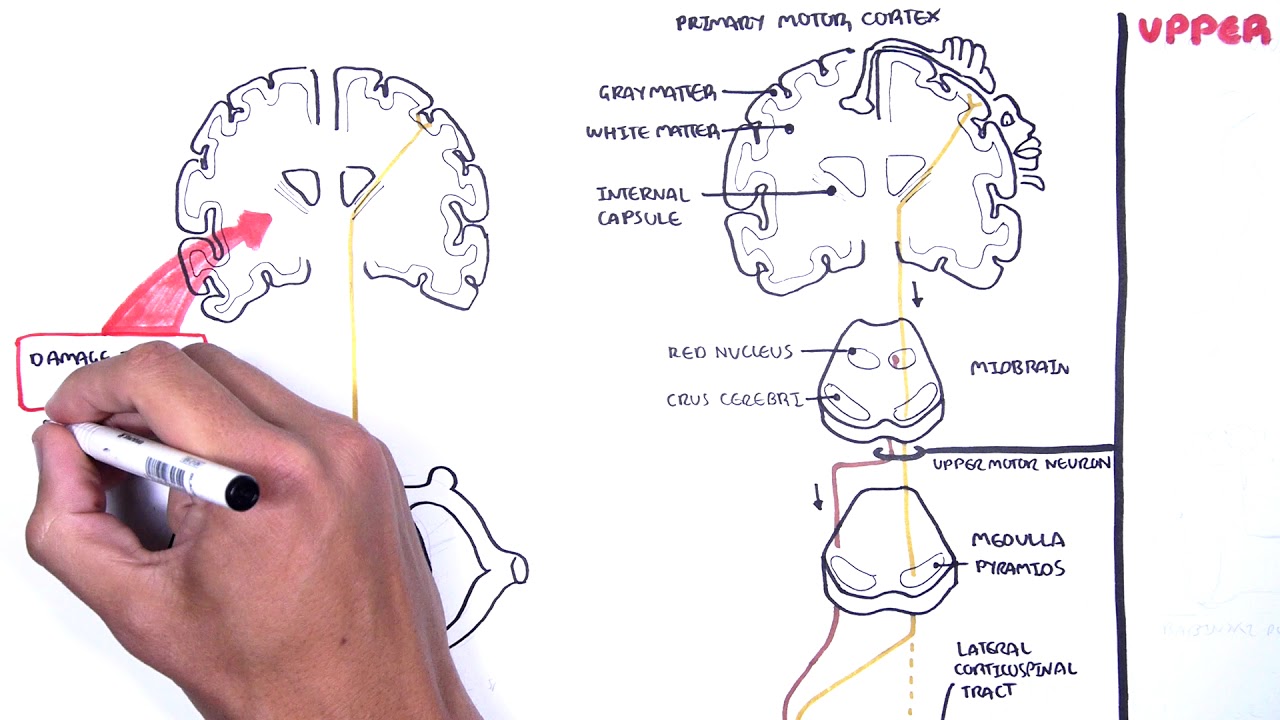
- 😀 Upper motor neurons start from the cortex and are divided into six anatomical levels: cortex, corona radiata, internal capsule, brainstem, spinal cord, and direct cells.
- 😀 Lower motor neurons involve the anterior horn cells, roots, plexus, nerves, neuromuscular junction, and muscles. LMN lesions are often categorized as polyneuropathy (multiple nerves involved) or mononeuropathy (one or a few nerves).
- 😀 Lesions in the cortex, corona radiata, and brainstem tend to present unilaterally, while spinal cord lesions can often be bilateral, particularly in conditions like cervical myelopathy or central cord syndrome.
- 😀 For bilateral proximal weakness, the main differential diagnoses include spinal cord lesions (e.g., cervical myelopathy), neuromuscular junction disorders, muscle diseases, and polyneuropathy.
- 😀 In muscle diseases like myopathies, weakness tends to be more proximal, and patients may not experience noticeable weakness in distal muscles due to their smaller size.
- 😀 Reflexes play a key role in diagnosis: hyperreflexia suggests an upper motor neuron lesion (e.g., spinal cord injury), while hyporeflexia or areflexia points towards a lower motor neuron disorder (e.g., polyneuropathy or myopathy).
- 😀 Sensory examination helps narrow down the diagnosis: normal sensation suggests a myopathy, while reduced sensation may point to a spinal cord lesion or polyneuropathy.
- 😀 A key philosophical question in neurology is why proximal muscles are often more affected in muscle diseases, with larger muscles being more susceptible to prominent symptoms despite distal muscles also being involved.
- 😀 When examining a patient with bilateral proximal weakness and wasting, it's important to rule out both upper and lower motor neuron causes, considering the location and distribution of symptoms to make an informed diagnosis.
Q & A
What are the primary distinctions between upper motor neuron and lower motor neuron lesions in limb examinations?
-Upper motor neuron lesions typically originate in the cortex and can affect areas like the corona radiata, internal capsule, brainstem, and spinal cord. They often present with unilateral findings. Lower motor neuron lesions, on the other hand, involve structures like the anterior horn cells, roots, plexus, nerves, neuromuscular junction, and muscles. They tend to present bilaterally and are associated with features like muscle wasting and weakness.
What is the significance of distinguishing between proximal and distal weakness in neurological examinations?
-The distinction between proximal and distal weakness helps localize the lesion. Proximal weakness is often seen in muscle and neuromuscular junction diseases, while distal weakness is more commonly seen in polyneuropathy or motor neuron diseases. Proximal muscles, due to their larger size, tend to show more prominent symptoms in diseases affecting the neuromuscular junction or muscles.
Why are larger muscles more likely to exhibit prominent symptoms in neuromuscular junction disorders?
-In neuromuscular junction disorders such as myasthenia gravis, larger muscles like the shoulder and thigh muscles exhibit more prominent symptoms due to their size. The smaller, distal muscles are still affected but are less noticeable because their weakness is not as obvious to the patient or on examination.
How does spinal cord involvement affect the presentation of limb weakness?
-Spinal cord lesions, particularly those in the cervical region (C5-C6), can lead to bilateral proximal weakness in the upper limbs. Conditions such as cervical myelopathy or central cord syndrome, like in syringomyelia, often present with weakness in the proximal muscles, with possible associated sensory loss in specific dermatomes (e.g., C5 and C6).
What are the primary conditions to consider when diagnosing bilateral proximal weakness with wasting?
-The main conditions to consider in the case of bilateral proximal weakness with wasting are spinal cord lesions (such as cervical myelopathy or syringomyelia), lower motor neuron diseases (like polyneuropathy or myopathies), and neuromuscular junction disorders. The clinical signs and progression help to narrow down the differential diagnosis.
How does the presence or absence of reflexes help differentiate between potential diagnoses?
-Reflexes are a critical part of diagnosing neurological conditions. Hyporeflexia or areflexia, especially in the upper limbs, suggests a peripheral nerve or polyneuropathy. If reflexes are preserved or exaggerated, it may point towards central nervous system involvement, such as spinal cord lesions. In the case of myopathy, reflexes are often normal.
What role does sensory examination play in the diagnosis of bilateral proximal weakness?
-Sensory examination helps confirm or rule out certain diagnoses. In cases of bilateral proximal weakness, a normal sensory exam suggests a primary muscle disorder (like myopathy). If there is reduced sensation, it might indicate a spinal cord or polyneuropathy issue, as these conditions often involve sensory pathways.
What is central cord syndrome, and how does it relate to the clinical presentation of bilateral proximal weakness?
-Central cord syndrome is a type of spinal cord injury that often results from damage to the central portion of the cervical spinal cord. This condition typically causes bilateral weakness in the upper limbs, particularly in the proximal muscles, and can be associated with sensory deficits in the upper limbs. It is often seen in conditions like syringomyelia and cervical myelopathy.
Why are muscle diseases like polymyositis considered in the differential diagnosis for proximal weakness and wasting?
-Muscle diseases like polymyositis are considered in the differential diagnosis because they often present with bilateral proximal weakness and muscle wasting. Polymyositis is an inflammatory muscle disease, and the presence of muscle biopsies or skin rashes (in dermatomyositis) can further support this diagnosis.
How do polyneuropathies such as CIDP present clinically, and what makes them a key consideration in cases of bilateral proximal weakness?
-Chronic inflammatory demyelinating polyneuropathy (CIDP) is a condition that presents with proximal and distal weakness, often with sensory involvement. CIDP can cause weakness that ascends from the distal to the proximal muscles, leading to bilateral proximal weakness. Reflexes are often reduced, and the condition typically affects the motor nerves more than sensory ones.
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级浏览更多相关视频

¡Vía CORTICOESPINAL y Síndromes de Motoneurona! PARA ESTUDIANTES

TRAKLINDAS 5 - PEMERIKSAAN NEUROLOGI REFLEKS
Introduction to Upper and Lower Motor Neuron Lesions

Lower Limb Neurological Examination | OSCE Guide | NEW | UKMLA | CPSA

Movement and Reflexes

Macleod s examination of the motor system of the lower limbs
5.0 / 5 (0 votes)
