Malnutrition in Hospitalized Patients
Summary
TLDRThis video provides an overview of malnutrition in hospitalized patients, focusing on undernutrition. It explores the definition of malnutrition by the WHO and its impact on patient outcomes, including complications like infections, longer hospital stays, and higher mortality rates. The video traces the history of malnutrition awareness, from Dr. Butterworth's 1974 paper to the development of modern screening and assessment tools. It highlights the importance of early detection, nutrition interventions, and standardized assessment practices in ensuring proper care, as well as the financial implications for hospitals in diagnosing malnutrition.
Takeaways
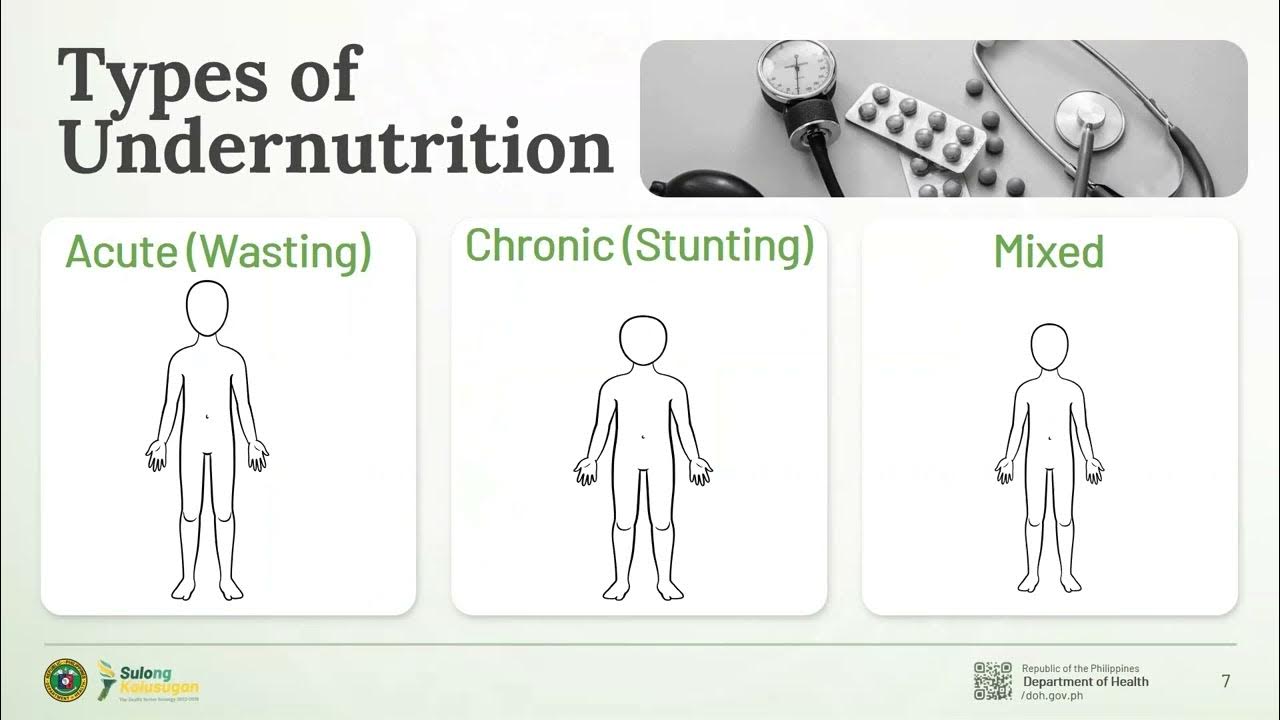
- 📊 Malnutrition includes both undernutrition and overnutrition, with the focus in hospitals primarily on undernutrition.
- 🌍 The World Health Organization defines malnutrition as deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients.
- 🏥 Undernutrition is a significant concern in hospitalized patients and can lead to worsened health outcomes and prolonged hospital stays.
- 📅 Since 1996, hospitals in the U.S. have been required to screen all admitted patients for malnutrition within the first 24 hours.
- 🛠️ Various screening tools like the Malnutrition Screening Tool (1999) and Nutrition Risk Screening (2002) have been developed to streamline early detection.
- 🔬 A comprehensive assessment for malnutrition includes medical history, physical examination, anthropometrics, and lab data, typically performed by dietitians.
- 📉 Malnutrition in hospitalized patients leads to muscle mass loss, impaired immune response, and delayed wound healing, increasing the risk of infections and complications.
- 💰 Accurate diagnosis and documentation of malnutrition can increase hospital reimbursement and justify the allocation of resources for better care.
- 📋 Recent trends emphasize the standardization of malnutrition assessment tools to ensure consistency in diagnosis and facilitate better research and education.
- ✔️ The Malnutrition Screening Tool (1999) and the etiology-based assessment tool from the Academy and Aspen (2012) are recommended for consistent screening and diagnosis across hospitals.
Q & A
What is the World Health Organization's definition of malnutrition?
-The World Health Organization defines malnutrition as deficiencies, excesses, or imbalances in a person's intake of energy and/or nutrients. This includes overnutrition (such as overweight and obesity) and undernutrition (a lack of essential nutrients).
Why is undernutrition a focal point in the context of hospitalized patients?
-Undernutrition is common among hospitalized patients and can have devastating consequences, including worse health outcomes, longer hospital stays, increased risk of infection, and delayed recovery. As a result, addressing undernutrition is a priority in clinical nutrition.
What was the significance of Dr. Charles E. Butterworth's 1974 paper 'The Skeleton in the Hospital Closet'?
-Dr. Butterworth's paper highlighted the widespread presence of unrecognized malnutrition in hospitals. He argued that malnutrition was a common issue among hospitalized patients due to neglect of nutrition in medical education and healthcare systems.
What is the purpose of the subjective global assessment (SGA) tool created in the 1980s?
-The subjective global assessment (SGA) tool was developed to classify patients as well-nourished, moderately malnourished, or severely malnourished. It is recognized as a valid and reliable tool for assessing malnutrition.
What role does the Joint Commission play in addressing malnutrition in hospitals?
-In 1996, the Joint Commission mandated that all hospitalized patients undergo nutrition screening within the first 24 hours of admission. This ensures early identification of those at risk for malnutrition and enables them to receive specialized nutrition care.
What are some examples of screening tools used to identify malnutrition in hospitals?
-Examples of malnutrition screening tools include the Malnutrition Screening Tool (1999), Nutrition Risk Screening 2002 (2002), Malnutrition Universal Screening Tool (2003), and Short Nutrition Assessment Questionnaire (2005).
Why is it important to diagnose and document malnutrition in the hospital's electronic medical record (EMR)?
-Diagnosing and documenting malnutrition in the EMR ensures that patients receive appropriate care and helps hospitals receive higher reimbursement for treatment. It also contributes to better resource allocation for malnourished patients.
What impact does malnutrition have on patient outcomes and hospital resources?
-Malnourished patients experience worse outcomes, such as longer hospital stays, higher readmission rates, and increased mortality. They also require more resources, including nutrition support, wound care, additional medications, and life-saving therapies.
How does the Academy of Nutrition and Dietetics recommend screening and assessing for malnutrition?
-The Academy recommends using the Malnutrition Screening Tool within the first 24 hours of hospital admission. If the patient's score is 2 or higher, they should undergo a full nutrition assessment using criteria established by the Academy and ASPEN in 2012, which include six clinical characteristics like energy intake and muscle loss.
What are the six clinical characteristics used in the malnutrition assessment tool created by the Academy and ASPEN?
-The six clinical characteristics are energy intake, weight loss, loss of subcutaneous fat, muscle loss, fluid accumulation, and reduced grip strength. A patient is diagnosed with malnutrition if they meet the criteria for at least two of these characteristics.
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级5.0 / 5 (0 votes)