Liver Function Tests - an overview
Summary
TLDR本视频由Dr. Matt主讲,深入探讨了肝功能测试(LFTs)的基本概念、为何需要进行这些测试以及如何解读测试结果。视频首先定义了肝功能测试作为血液生物标志物,用以评估肝脏功能。接着,通过实例解释了可能需要进行肝功能测试的情况,如患者有肝病史、黄疸症状、药物中毒风险或家族肝病史。最后,视频通过图解详细说明了如何通过肝功能测试结果判断黄疸的原因,以及肝功能障碍的两大类别:胆汁淤积(胆固醇排泄问题)和肝细胞损伤(肝脏本身的问题)。
Takeaways
- 🧬 肝功能测试是通过血液生物标志物来评估肝脏是否正常工作的一种方法。
- 🩸 常见的肝功能测试包括酶类(如AST、ALT、ALP、GGT)和肝脏产生的产物(如白蛋白、凝血酶原时间、胆红素)。
- 📈 肝功能测试可能因为多种原因被要求进行,例如患者有肝病史、黄疸症状、药物或酒精使用史,或者属于高风险群体。
- 🔍 肝功能测试结果异常可能指示肝脏损伤或疾病,或者是肝脏功能不全。
- 🟠 黄疸是皮肤和黏膜出现黄色着色,通常是由于胆红素积累造成。
- 🩸 胆红素是红细胞分解的产物,主要在肝脏中被处理和排泄。
- 💡 通过肝功能测试可以区分黄疸的原因,如前肝源性(红细胞破坏增加)、肝内源性(排泄障碍)和后肝源性(胆汁排泄问题)。
- 📊 碱性磷酸酶(ALP)和γ-谷氨酰转移酶(GGT)的升高通常表明胆汁排泄受阻,即胆道阻塞。
- 🚨 AST和ALT的显著升高可能指示急性肝损伤,而轻微升高可能与慢性影响有关。
- 🍺 AST相对于ALT的升高可能与酒精性肝病有关,而两者比例的变化也可能指示肝硬化。
- 📉 肝脏功能不全时,白蛋白和凝血因子的产生会减少,同时胆红素的处理也会受到影响。
Q & A
肝脏功能测试是什么?
-肝脏功能测试是血液参数,也称为血液生化标志物,用于指示肝脏可能没有正常工作。
AST和ALT的区别是什么?
-AST(天门冬氨酸氨基转移酶)和ALT(丙氨酸氨基转移酶)都是指示肝脏损伤的酶。AST主要存在于线粒体中,而ALT主要存在于细胞质中。在血液中,这两种酶的比例大约是1:1。
为什么ALT比AST更特异于肝脏损伤?
-ALT主要存在于肝细胞的细胞质中,因此当肝脏损伤时,ALT的水平会比AST更显著地升高,使其成为更特异于肝脏损伤的指标。
ALP和GGT在肝脏功能测试中的作用是什么?
-ALP(碱性磷酸酶)和GGT(γ-谷氨酰转移酶)在肝脏功能测试中用于指示胆道阻塞或胆汁淤积。ALP的增加可能与肝脏外部的骨组织有关,而GGT的增加则更特异地指示肝脏问题。
黄疸是如何产生的?
-黄疸是由于血液中胆红素积累导致的,表现为皮肤和黏膜的黄染。胆红素是红细胞分解的产物,在肝脏中被代谢和排泄。
如何区分黄疸的前肝性和后肝性原因?
-前肝性黄疸通常与红细胞破坏增加有关,导致间接胆红素(未结合胆红素)水平升高。后肝性黄疸则与胆汁排泄障碍有关,导致直接胆红素(结合胆红素)水平升高。
肝脏功能测试中的凝血因子和白蛋白有什么意义?
-凝血因子和白蛋白是肝脏产生的产品,它们的水平可以反映肝脏的合成功能。如果这些水平低于正常范围,可能表明肝脏功能受损。
肝脏功能测试可能因为哪些原因被要求进行?
-肝脏功能测试可能因为患者有肝病史、黄疸、药物或毒物暴露史、家族肝病史、高风险群体筛查(如血液透析、病毒性肝炎暴露、药物滥用史)或疑似肝脏损伤的其他原因而被要求进行。
肝脏细胞损伤时,AST和ALT水平的变化意味着什么?
-如果AST和ALT水平显著升高(超过正常值的10倍),通常意味着有急性严重的肝脏炎症。如果水平升高较轻(约5倍),则可能表明是慢性肝脏损伤。
肝脏功能测试中的胆红素水平变化指示了什么?
-胆红素水平的变化可以指示肝脏在处理和排泄胆红素方面是否存在问题。胆红素水平的升高可能与肝脏损伤、胆道阻塞或红细胞破坏增加有关。
如何通过肝脏功能测试判断是否存在胆汁淤积?
-如果ALP和GGT水平升高,且直接胆红素水平也升高,这可能表明存在胆汁淤积。胆汁淤积可能是由于胆道阻塞或其他影响胆汁排泄的因素导致的。
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级浏览更多相关视频
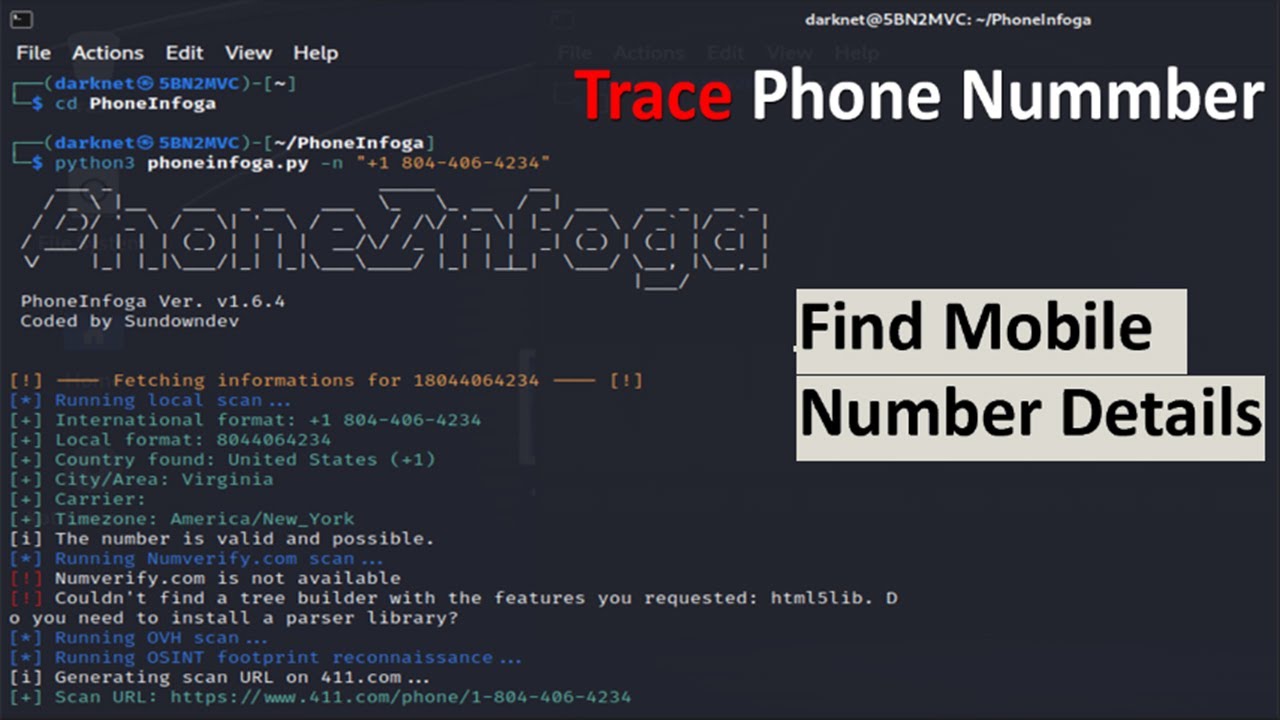
How To Find Mobile Number Details || Advanced Kali Linux Tool

【東方】Bad Apple!! PV【影絵】

INDIAN BURGER | VADA PAV | Indian Street Food Recipe Making in Village | Rainy Day Cooking

Festo – BionicSoftHand

SIBO: A doctor's guide to the root cause of Bloating and IBS

KEFAI Automatic Desktop Bottle Filing, Capping And Labeling Machine Line

客户开发 | 外贸客户开发之主动开发,只需四步,从此不再缺订单 | 国际贸易
5.0 / 5 (0 votes)