No one should die because they live too far from a doctor | Raj Panjabi
Summary
TLDRThe speaker recounts his journey from a war-torn childhood in Liberia to becoming a doctor in America, emphasizing the lesson 'no condition is permanent.' He founded Last Mile Health, a nonprofit that trains community health workers in remote areas, leveraging technology to bridge the gap in healthcare access. The speaker's TED Prize wish is to create the Community Health Academy, a global platform for training these workers, aiming to save millions of lives by 2030.
Takeaways
- 🌟 The speaker's father instilled in him the belief that 'no condition is permanent', a lesson that has profoundly influenced his life.
- 🏞️ Growing up in Monrovia, Liberia, the speaker had a privileged childhood until the outbreak of civil war in 1989 disrupted his life.
- 🚁 Forced to flee due to the war, the speaker and his family were among the fortunate ones to escape on a rescue plane, leaving many behind.
- 🏡 Resettling in America, the speaker's family received support from a community that helped them rebuild their lives.
- 🎓 The mantra 'no condition is permanent', along with community support, enabled the speaker to pursue higher education and become a doctor.
- 🏥 Returning to Liberia as a medical student, the speaker was shocked by the severe lack of healthcare, with only 51 doctors for a population of four million.
- 🌐 Recognizing the global issue of inaccessible healthcare in remote communities, the speaker was determined to address this disparity.
- 👩⚕️ The speaker introduced the concept of community health workers, like Musu, who could bridge the gap in healthcare access in rural areas.
- 🤝 The nonprofit organization Last Mile Health was founded to train, equip, and pay community health workers, thereby improving healthcare delivery.
- 📱 Technology, including smartphones and medical tests, was integrated to empower community health workers and enhance their capabilities.
- 🌟 The speaker's TED Prize wish is to create the Community Health Academy, a platform to train and connect community health workers worldwide.
Q & A
What is the central lesson the speaker learned from his father?
-The central lesson the speaker learned from his father is that 'no condition is permanent,' which means that circumstances can change and one should not be defined by their current situation.
Why did the speaker's family have to flee from Liberia?
-The speaker's family had to flee from Liberia due to the civil war that erupted in 1989, which led to the closure of schools and panic among the citizens as rebel armies approached their hometown.
How did the community in America support the speaker's family after their arrival?
-The community in America supported the speaker's family by taking them into their homes, mentoring the speaker, and helping his father start a clothing shop.
What was the impact of the civil war on Liberia's healthcare system?
-The civil war left Liberia with just 51 doctors to serve a population of four million people, highlighting a severe lack of healthcare professionals, especially in rural areas.
What is the 'Last Mile Health' initiative the speaker co-founded?
-Last Mile Health is a nonprofit co-founded by the speaker, aimed at bringing a health worker within reach of every person, everywhere by training, equipping, and paying community health workers to serve their local communities.
How does the speaker propose to use technology to improve training for community health workers?
-The speaker proposes to use technology to create a global platform, the Community Health Academy, which will provide digital education resources to train community health workers more effectively and efficiently.
What was the speaker's TED Prize wish?
-The speaker's TED Prize wish was to recruit the largest army of community health workers the world has ever known by creating the Community Health Academy, a platform to train, connect, and empower them.
How did the Ebola outbreak in 2013 highlight the importance of community health workers?
-The Ebola outbreak in 2013 highlighted the importance of community health workers as they played a crucial role in identifying symptoms, tracking the virus, and breaking the chain of transmission, demonstrating their value in emergency situations.
What is the potential impact of training community health workers in 75 countries as mentioned in the script?
-Training community health workers in 75 countries could save the lives of nearly 30 million people by 2030 by providing essential healthcare services in remote and underserved areas.
How does the speaker's personal experience with his wife's pregnancy relate to the importance of community health workers?
-The speaker's personal experience of hearing his baby's heartbeat during his wife's pregnancy parallels the joy and importance of prenatal care. He contrasts this with a woman in Liberia who had no access to such care until community health workers were trained, emphasizing the life-changing impact of their work.
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级浏览更多相关视频

Finding your coping mechanism | Joseph Lewis | TEDxFoggyBottom
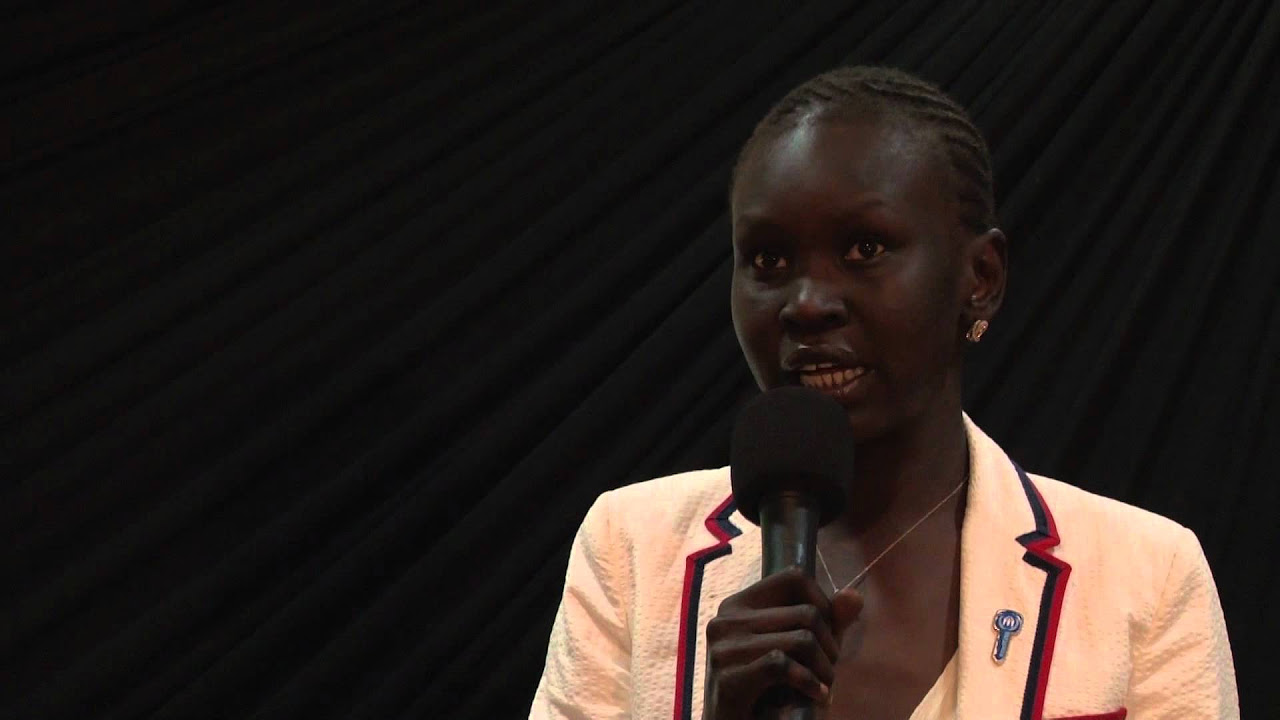
Education: The Key to South Sudan's Success: Alek Wek at TEDxJuba

TIMAWA| BAHAGI NG NOBELA NI AGUSTIN FABIAN| ARALIN SA FILIPINO

Tackling ethnic health disparities: Lisa Cooper at TEDxBaltimore 2014

The Moth: Go Tell It on the Mountain - Jim Gates

Ben Carson on the power of the mind
5.0 / 5 (0 votes)
