Mechanism of Diabetic dyslipidemia made easy
Summary
TLDRThis talk delves into diabetic dyslipidemia, a condition characterized by increased triglycerides, elevated VLDL, small dense LDL particles, and reduced HDL levels, all contributing to heightened cardiovascular risk in diabetics. It explains the role of insulin resistance in increasing free fatty acids, which in turn affects liver function and leads to a cascade of metabolic issues, including atherosclerosis and unstable plaques, emphasizing the vicious cycle of dyslipidemia in diabetes.
Takeaways
- 🚨 Diabetic dyslipidemia is characterized by four main components: increased triglycerides, increased VLDL, increased small dense LDL particles, and reduced HDL levels, all contributing to heightened cardiovascular risk in diabetic patients.
- 🔬 Triglycerides are stored in adipose tissue as a less toxic form of free fatty acids and are broken down by lipase into free fatty acids and glycerol.
- 🌡 Insulin plays a crucial role in regulating lipase activity, preventing the breakdown of triglycerides into free fatty acids, which is a key process in managing dyslipidemia.
- 🔄 Insulin resistance, a hallmark of diabetes, leads to increased lipase activity and consequently, higher levels of free fatty acids in the blood.
- 🔄 The vicious cycle of increased free fatty acids further exacerbates insulin resistance, contributing to the dyslipidemia associated with diabetes.
- 🏗️ The liver, as a central player, converts the increased free fatty acids into triglycerides, which can lead to non-alcoholic fatty liver disease and hepatic insulin resistance.
- ➡️ The liver's response to increased triglycerides includes packaging them into VLDL particles, which are released into the bloodstream and contribute to the dyslipidemia.
- 🔄 VLDL particles are converted to IDL and then to LDL, particularly small and dense LDL particles that are prone to deposit in blood vessels and cause atherosclerosis.
- ⚠️ The process of cholesterol ester transfer protein (CETP) facilitates the exchange of triglycerides from VLDL and LDL to HDL and cholesterol back, reducing HDL levels.
- 🛑 The reduction in HDL levels is due to its increased triglyceride content, which attracts hepatic lipase to break down HDL, further contributing to the dyslipidemia.
- 🔄 LDL particles in diabetic dyslipidemia are not only small and dense but also more prone to oxidation and glycation, leading to unstable plaques and increased risk of cardiovascular events.
Q & A
What is diabetic dyslipidemia?
-Diabetic dyslipidemia is a condition characterized by an abnormal lipid profile in patients with diabetes, which includes increased triglycerides, increased VLDL, increased small dense LDL particles, and reduced HDL levels. These components contribute to an increased cardiovascular risk.
What are the four main components of diabetic dyslipidemia?
-The four main components of diabetic dyslipidemia are increased triglycerides, increased VLDL (very-low-density lipoprotein), increased small dense LDL (low-density lipoprotein) particles, and reduction of HDL (high-density lipoprotein).
What is the role of lipase in the context of diabetic dyslipidemia?
-Lipase is an enzyme that breaks down triglycerides into free fatty acids and glycerol. In diabetic dyslipidemia, the action of lipase is inhibited by insulin, preventing the breakdown of triglycerides. However, insulin resistance can lead to increased lipase activity, resulting in higher levels of free fatty acids in the blood.
How does insulin resistance affect the process of lipase activity and triglyceride breakdown?
-Insulin resistance impairs the ability of insulin to inhibit lipase activity. As a result, lipase becomes more active, leading to increased breakdown of triglycerides into free fatty acids and glycerol, which contributes to the dyslipidemia seen in diabetes.
What is the significance of increased free fatty acids in the bloodstream in diabetic dyslipidemia?
-Increased free fatty acids in the bloodstream can create a vicious cycle by further increasing insulin resistance. This leads to more lipase activity, more breakdown of triglycerides, and ultimately, a higher production of triglycerides in the liver.
How does the liver contribute to diabetic dyslipidemia?
-The liver plays a significant role in diabetic dyslipidemia by increasing triglyceride production due to the influx of free fatty acids. This leads to either increased storage of triglycerides in the liver, contributing to non-alcoholic fatty liver disease, or packaging of triglycerides into VLDL particles that are released into the bloodstream.
What is the process of VLDL conversion to LDL in the context of diabetic dyslipidemia?
-In diabetic dyslipidemia, the increased triglycerides produced in the liver are packaged into VLDL particles and released into the bloodstream. VLDL is then converted to IDL (intermediate-density lipoprotein), which in turn is converted to LDL. This process results in an increase of small and dense LDL particles.
Why are small and dense LDL particles problematic in diabetic dyslipidemia?
-Small and dense LDL particles are problematic because they tend to get deposited more in the blood vessels, leading to atherosclerosis. This increases the risk of cardiovascular diseases in diabetic patients.
How does the cholesterol ester transfer protein (CETP) affect HDL levels in diabetic dyslipidemia?
-CETP facilitates the transfer of triglycerides from VLDL and LDL to HDL, while taking up cholesterol from HDL. This exchange results in HDL becoming enriched with triglycerides, which are then more likely to be taken up by the liver and broken down, leading to a reduction in HDL levels.
What are the consequences of reduced HDL levels in diabetic dyslipidemia?
-Reduced HDL levels in diabetic dyslipidemia mean less of the protective cholesterol is available to remove LDL from the bloodstream. This can lead to an accumulation of LDL in the arteries, contributing to atherosclerosis and increasing cardiovascular risk.
How do increased oxidation and glycation of LDL contribute to atherosclerosis in diabetic dyslipidemia?
-Increased oxidation of LDL produces unstable plaques that are more prone to rupture, increasing the risk of coronary artery disease or acute events like myocardial infarction or stroke. Glycation of LDL, due to high glucose levels, alters its structure, making it less recognizable by LDL receptors and leading to increased circulatory time and deposition in the arteries, further promoting atherosclerosis.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Physiology of Lipoproteins Cholesterol

LIPOPROTEÍNAS - QUILOMÍCRONS, VLDL, LDL E HDL

Lipoprotein metabolism and transport | Chylomicron, VLDL,IDL, LDL,HDL | Metabolism | Biochemistry

Kimia Klinik: Analisis Lipid dan Lipoprotein
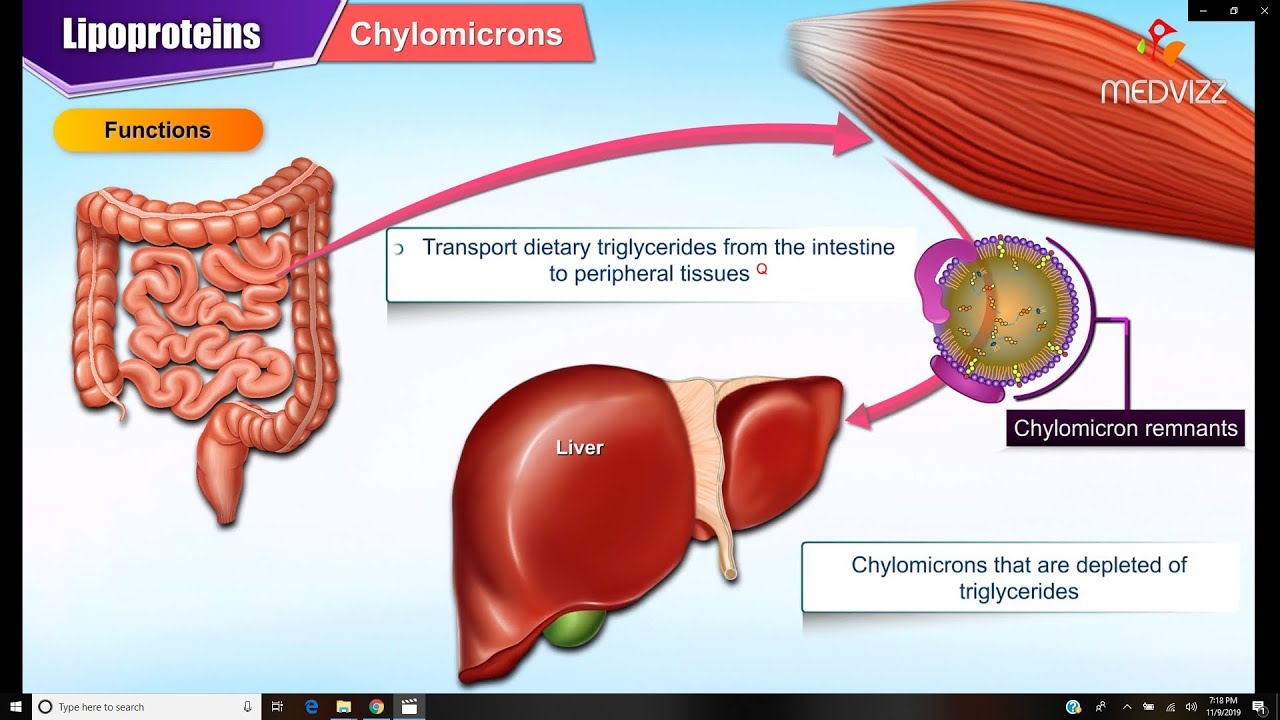
Lipoproteins and Apolipoproteins - Structure , function and metabolism : Medical Biochemistry

Dr. Paul Mason - 'The truth about high cholesterol'
5.0 / 5 (0 votes)