B-Cell Activation and Function
Summary
TLDRThis video explains the activation and function of B cells in the adaptive immune system. It details how B cells encounter pathogens, use B cell receptors to bind antigens, endocytose pathogens, and present peptides on MHC class II molecules. These B cells then interact with helper T cells, receive signals to produce antibodies, and undergo processes like isotype switching and somatic hypermutation. The end result is the production of highly effective antibodies by plasma cells, which help eliminate infections.
Takeaways
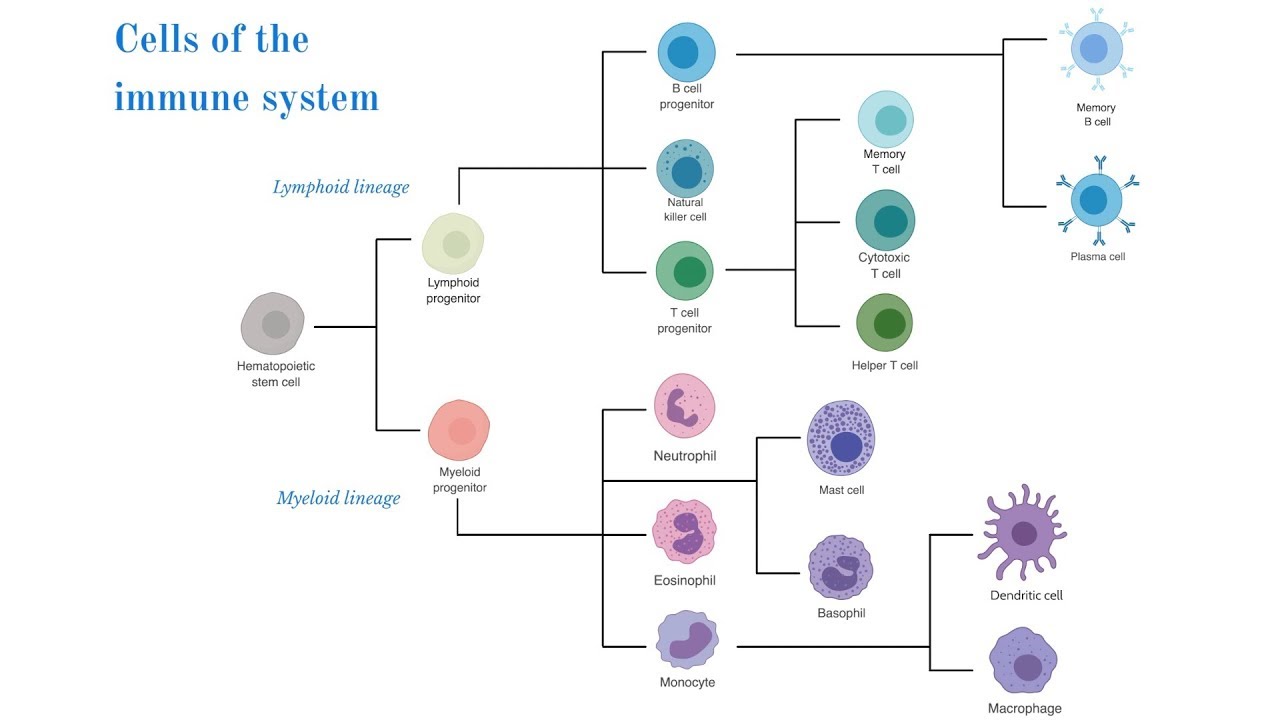
- 🔬 T-cells are unique cells in the adaptive immune system with specific functions that require full activation.
- 🦠 Once T-cells encounter a signal through an antigen-presenting cell (APC), they signal B-cells to find and neutralize the pathogen.
- 🧬 B-cells use a B-cell receptor (BCR) to bind to an antigen on the pathogen's surface, leading to endocytosis of the pathogen.
- 🔗 The pathogen is broken down into peptides, which bind with MHC class II molecules and are presented on the B-cell surface.
- 🧪 The B-cell travels to secondary immune tissues, like lymph nodes, and interacts with helper T-cells, presenting the MHC-peptide complex.
- 📡 The interaction of MHC with T-cell receptors and CD4 co-receptors confirms the presence of a pathogen, leading to the release of cytokines, including IL-4.
- 💉 IL-4 binds to the B-cell receptor, signaling it to produce antibodies to neutralize the pathogen, resulting in full B-cell activation.
- 🛡️ Activated B-cells produce IgM antibodies, the initial response to infection, which later improve through isotype switching to IgG antibodies for better pathogen targeting.
- 🔄 The quality of antibodies improves through somatic hypermutation, enhancing the adaptive immune response.
- 🧫 Activated B-cells replicate, with the best antibody-producing cells undergoing clonal selection, leading to plasma cells that continuously produce and secrete antibodies until the threat is eliminated.
Q & A
What is the main function of T-cells in the adaptive immune system?
-T-cells have specific functions in the adaptive immune system, such as signaling B-cells to find and neutralize pathogens after encountering an antigen through an antigen-presenting cell (APC).
How do B-cells become fully activated?
-B-cells become fully activated when they encounter a pathogen, use their B-cell receptor (BCR) to bind to an antigen on the pathogen's surface, endocytose the pathogen, process it, and present its peptides with MHC class II molecules on their surface. They then interact with helper T-cells and receive signals through the binding of CD40 ligand and the release of cytokines like IL-4.
What role does IL-4 play in B-cell activation?
-IL-4, released by helper T-cells, binds to receptors on B-cells, signaling them to begin producing antibodies to neutralize the pathogen, leading to full activation of the B-cells.
What is the significance of IgM antibodies in an infection?
-IgM antibodies are the first antibodies produced during an infection. They are the least specific but provide an initial response to the infection. As the infection progresses, more specific antibodies are produced.
What is isotype switching in B-cells?
-Isotype switching is a process where the constant region of the antibody and BCR changes to produce antibodies that are better equipped to bind to the specific pathogen. For example, antibodies can switch from IgM to IgG, which are more effective against extracellular pathogens.
What is the role of activation-induced cytidine deaminase (AID) in antibody production?
-AID aids in the production of better antibodies by facilitating isotype switching and somatic hypermutation, which enhances the binding affinity of antibodies to the pathogen.
How does clonal selection improve the immune response?
-Clonal selection ensures that B-cells producing the best antibodies are selected to replicate more often. This leads to future generations of B-cells and antibodies that are better adapted to fight the specific pathogen.
What is the final stage of B-cell differentiation?
-The final stage of B-cell differentiation is becoming fully differentiated plasma cells. These cells specialize in producing and secreting antibodies to eliminate the pathogen.
What is the role of plasma cells in the immune response?
-Plasma cells are specialized cells whose sole function is to produce and secrete antibodies continuously until the pathogen is eliminated.
Why is somatic hypermutation important for B-cell function?
-Somatic hypermutation increases the mutation rate in the variable regions of antibodies and BCRs, leading to the production of antibodies with higher affinity for the pathogen. This process improves the quality of the immune response.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade Now5.0 / 5 (0 votes)