What makes a Team Teams and teamwork in healthcare 5/7
Summary
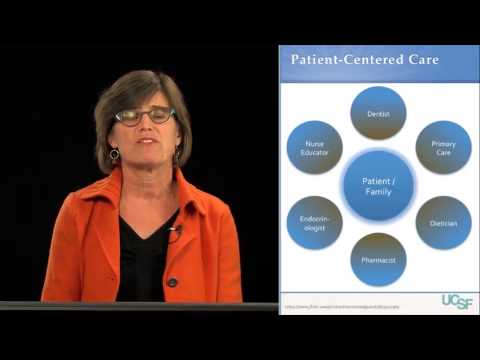
TLDRThis segment explores the dynamics of team-based healthcare, highlighting the importance of interprofessional collaboration. It outlines the key features of effective teams, such as shared identity, goals, and responsibilities, and discusses the varying degrees of interprofessional interaction from teamwork to coordination. Barriers and facilitators to collaboration are also examined, emphasizing the need for communication skills, shared competencies, and supportive infrastructure.
Takeaways
- 😀 The segment focuses on understanding what makes a team in healthcare, emphasizing the importance of interprofessional collaboration.
- 🏥 Teams in healthcare can vary, from resuscitation teams in hospitals to surgical teams in operating rooms to primary care teams in outpatient clinics.
- 🔑 Key features of teams include a shared identity, shared goals, shared responsibility, interdependence, and the ability to act and make decisions autonomously.
- 👩⚕️👨⚕️ Team membership in healthcare often changes over time, requiring flexibility and adaptability among team members.
- 🏠 An example of a healthcare team is the Acute Care for Elders (ACE) unit at San Francisco General Hospital, aiming to return hospitalized older adults back home.
- 🤝 Interprofessional work in healthcare can take various forms, including teamwork, collaboration, and coordination, each requiring different levels of connection and shared identity.
- 📚 Scott Reeves' framework in his book on interprofessional teamwork in healthcare helps understand how healthcare professionals work together.
- 🤔 Barriers to interprofessional collaboration include a lack of critical skills in communication and teamwork, training in silos, and existing infrastructures that do not support collaboration.
- 🏢 Existing reimbursement structures often do not foster interprofessional collaboration, posing a challenge to more integrated care.
- 💡 Facilitators of interprofessional collaboration include patient characteristics, shared competency between professions, efficiencies from collaborative work, and policy issues driving towards collaborative practice.
- 📈 The segment encourages reflection on observed types of interprofessional work in one's own setting and understanding the dynamics of teamwork, collaboration, and coordination.
Q & A
What is the main focus of segment five of the video?
-The main focus of segment five is to explore what makes a team effective in healthcare, discussing team features, the framework for interprofessional collaboration, and the barriers and facilitators of such collaboration.
What are the key features of teams in healthcare as described in the literature?
-Key features of healthcare teams include a shared identity and goals, shared responsibility for achieving these goals, defined but potentially changing team membership, interdependence among team members, and the authority to act and make autonomous decisions.
How does team membership in healthcare often change over time and what is the challenge it presents?
-Team membership in healthcare often changes due to various factors such as staff rotation or patient case changes. The challenge it presents is ensuring that team members can work together effectively to achieve goals despite these changes.
What is an example of a team in healthcare and what are its goals?
-An example is the Acute Care for Elders (ACE) team at San Francisco General Hospital, whose goal is to return hospitalized older adults back home by maintaining their physical function during hospital stay and avoiding complications.
What roles do the members of the ACE team play in achieving their goals?
-The ACE team consists of bedside nurses, occupational therapists, nutritionists, pharmacists, a social worker, a clinical nurse specialist, and a physician, all working together to provide comprehensive care for older adults.
What is the difference between teamwork, collaboration, and coordination as forms of interprofessional work?
-Teamwork requires a high degree of coordination and shared identity among members. Collaboration involves shared accountability and some interdependence with less predictable team goals and roles. Coordination is the loosest form, where healthcare professionals work independently with less integration and interdependence.
According to Scott Reeves' framework, what are the looser forms of interprofessional work?
-The looser forms of interprofessional work, as described by Scott Reeves, include collaboration and coordination, where there is less shared identity and integration of members compared to teamwork.
What are some examples of interprofessional collaboration and coordination mentioned in the script?
-An example of interprofessional collaboration is a team in a large general medicine ward, where various healthcare professionals communicate about patient care. An example of coordination is a sports medicine practice working alongside a physical therapy group, communicating mainly when necessary.
What are some of the barriers to interprofessional collaboration in healthcare?
-Barriers to interprofessional collaboration include a lack of critical skills in communication and teamwork, training in silos leading to different professional values and perspectives, infrastructure issues like schedules and lack of rewards, and existing reimbursement structures that do not foster collaboration.
What are the driving forces moving healthcare towards interprofessional collaboration?
-The driving forces include patient characteristics, shared competencies between professions, efficiencies from collaborative work, and policy issues that encourage a more collaborative practice.
How can understanding the different forms of interprofessional work help healthcare professionals?
-Understanding the different forms of interprofessional work can help healthcare professionals identify the level of connection and coordination required in their specific setting, allowing them to better structure their collaborative efforts and improve patient care.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

What is interprofessional collaborative practice 1/7

Why does interprofessional collaboration matter The Triple Aim in Healthcare 3/7
How does interprofessional collaboration impact care The patient 's perspective 2/7

IPE Core Competency Domain 4: Teams and Teamwork

Ethical Interprofessional Collaboration

VIDEO ROLE PLAY PENERAPAN IPE DAN IPC DALAM PELAYANAN KESEHATAN
5.0 / 5 (0 votes)