Appendicitis: Introduction, Pathogenesis, Cllinical features, Lab findings, Imaging, Management
Summary
TLDRThis video provides an in-depth overview of acute appendicitis, including its pathogenesis, clinical presentation, lab findings, imaging techniques, and management strategies. Appendicitis is a common cause of acute abdominal pain, with a higher occurrence in individuals aged 10-30. The condition typically starts with inflammation in the appendix, which can lead to complications like perforation and peritonitis. Key symptoms include abdominal pain, nausea, and vomiting, while diagnostic methods like blood tests and imaging are used to confirm the condition. Treatment primarily involves appendectomy, with specific protocols based on whether the appendix is perforated or not.
Takeaways
- 😀 Appendicitis is a common cause of acute abdominal pain and one of the most frequent abdominal surgical emergencies, affecting up to 1 in 10 individuals.
- 😀 It most commonly presents between the ages of 10 and 30 years and has a slight male predominance, with a male-to-female ratio of 3:2 before age 30.
- 😀 The primary cause of appendicitis is appendiceal obstruction, often caused by fecaliths, lymphoid hyperplasia, or neoplasia, leading to increased pressure, thrombosis, and bacterial overgrowth.
- 😀 Pathogenesis involves obstruction, leading to an increase in intraluminal pressure, thrombosis, ischemia, and eventually perforation, which causes peritonitis.
- 😀 The classic clinical presentation includes right lower quadrant abdominal pain, anorexia, nausea, vomiting, and local tenderness, especially at McBurney's point.
- 😀 Key diagnostic signs include McBurney's point tenderness, Rovsing's sign, and the obturator and psoas signs, which help localize the inflamed appendix.
- 😀 Differential diagnoses for acute appendicitis include diverticulitis, ectopic pregnancy, nephrolithiasis, pelvic inflammatory disease, and ovarian torsion.
- 😀 Laboratory findings typically show leukocytosis, with an elevated white blood cell count and a left shift, indicating the presence of an inflammatory process.
- 😀 Imaging modalities like CT and ultrasound can help diagnose appendicitis, with CT showing an enlarged appendix with wall thickening, fat stranding, and possible appendicolith.
- 😀 The treatment of acute appendicitis typically involves appendectomy, with management differing based on whether the appendix is perforated or non-perforated, and the patient's clinical stability.
Q & A
What is acute appendicitis?
-Acute appendicitis is the inflammation of the vermiform appendix, commonly causing acute abdominal pain and requiring surgical intervention. It is one of the most frequent abdominal emergencies.
What are the common causes of acute appendicitis?
-The primary causes of acute appendicitis include obstruction of the appendix, often by a fecal lith (hard stool), lymphoid hyperplasia (common in children), or neoplasms in older patients.
What age group is most affected by appendicitis?
-Appendicitis most commonly affects individuals between the ages of 10 and 30, though it can occur in any age group.
What is the pathogenesis of appendicitis?
-Appendicitis begins with obstruction of the appendix, leading to increased pressure, thrombosis of small vessels, and bacterial overgrowth. In children, viral infections may cause lymphoid hyperplasia, while adults often have fecal lith obstruction.
How does appendicitis typically present in patients?
-The typical presentation of appendicitis includes abdominal pain that starts in the epigastric region and shifts to the right lower quadrant, along with symptoms like anorexia, nausea, vomiting, and rebound tenderness.
What are some classic signs of appendicitis on physical examination?
-Classic signs include McBurney's point tenderness, Rovsing's sign, Psoas sign, and Obturator sign, all indicating inflammation of the appendix or local peritoneal irritation.
What laboratory findings are common in acute appendicitis?
-Most patients with acute appendicitis show mild leukocytosis, with an elevated white blood cell count and a left shift, indicating the presence of immature neutrophils. Bilirubin levels may rise in cases of perforation.
What imaging techniques are used to diagnose appendicitis?
-The standard imaging methods for diagnosing appendicitis include abdominal CT with contrast and ultrasound. CT can identify an enlarged appendix, wall thickening, fat stranding, and appendicolith. Ultrasound is useful, especially in children, with a diameter of 6mm or more being indicative.
What is the definitive treatment for appendicitis?
-The definitive treatment for acute appendicitis is appendectomy, a surgical procedure to remove the inflamed appendix.
How is perforated appendicitis managed differently from non-perforated appendicitis?
-For perforated appendicitis, management includes urgent appendectomy, intravenous antibiotics (3-5 days), and in some cases, percutaneous drainage of abscesses. Non-perforated appendicitis may be managed with surgery or intravenous antibiotics if surgery is not possible.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Acute Pancreatitis: pathogenesis, clinical findings, and complications
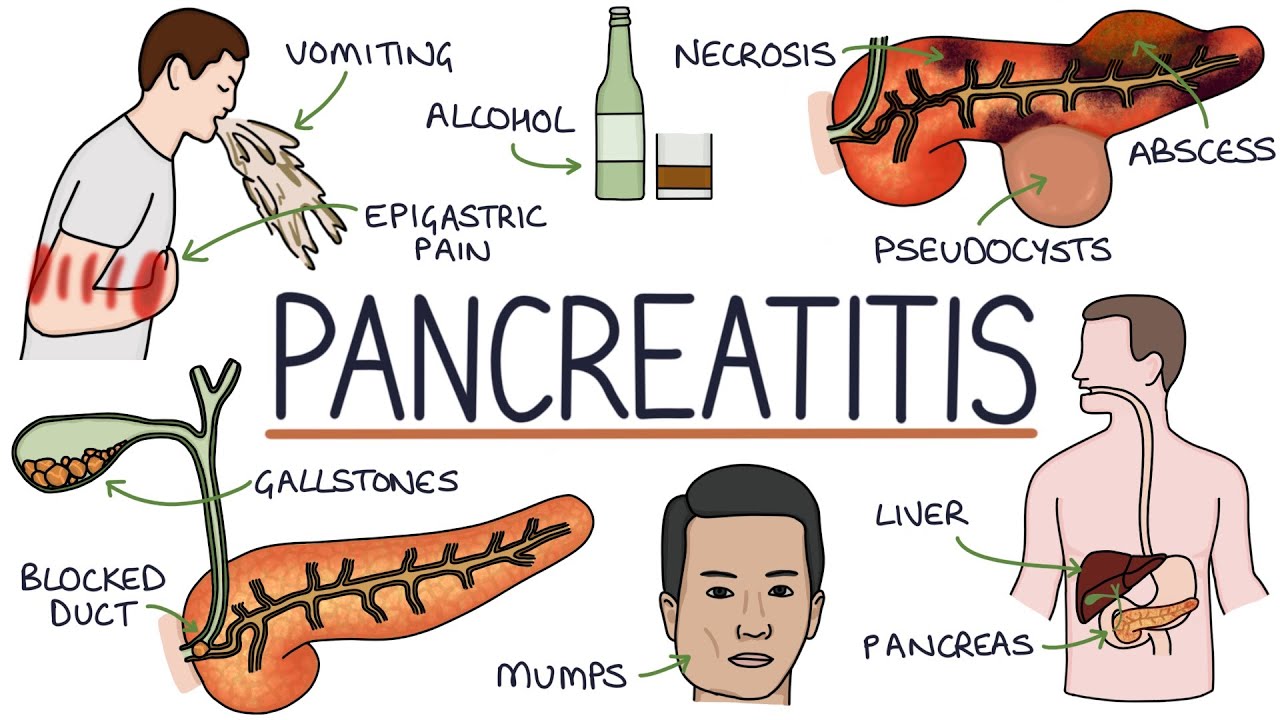
Understanding Pancreatitis

Renal Failure, Chronic Kidney Disease l End Stage Renal Disease for Nursing Exams, NCLEX RN & LPN
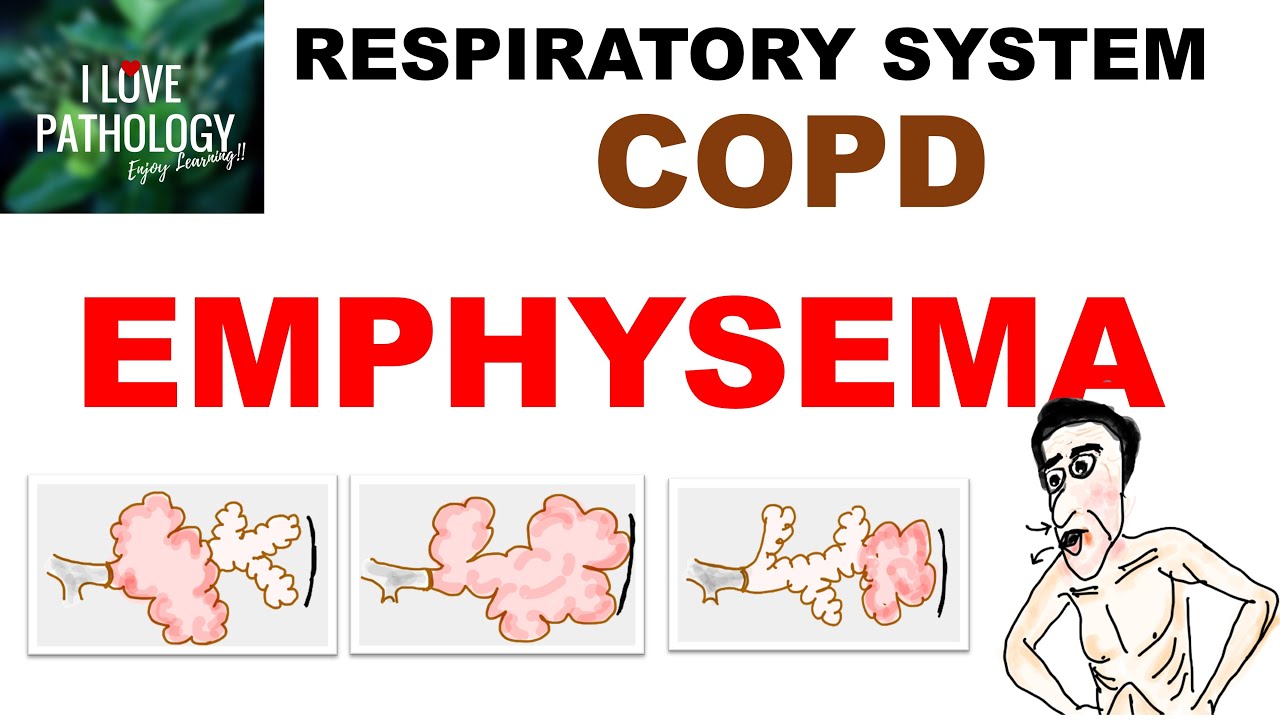
Chronic Obstructive Pulmonary Disease Part 1: Emphysema- Pathology

Persentasi ppt “APPENDICITIS konsep dan askep”

Diarrhea by M. Baskind, B. Hron, C. Callas, H. Moulton, A. Onate | OPENPediatrics
5.0 / 5 (0 votes)