Pharmacology - ANTICOAGULANTS & ANTIPLATELET DRUGS (MADE EASY)
Summary
TLDRThis lecture provides a comprehensive overview of anticoagulants, antiplatelet agents, and thrombolytics, focusing on their mechanisms of action, uses, and side effects. It covers platelet aggregation inhibitors like aspirin, P2Y12 blockers, and glycoprotein 2b/3a inhibitors, which prevent clot formation, as well as anticoagulants like heparin, warfarin, and direct thrombin inhibitors that disrupt the coagulation cascade. The lecture also highlights thrombolytics, which dissolve existing clots. The key risks, including bleeding and drug interactions, are discussed, making this an essential resource for understanding blood clot management in cardiovascular medicine.
Takeaways
- 😀 Anticoagulants and antiplatelet agents are used to treat thrombotic disorders, preventing blood clots that can cause heart attacks or strokes.
- 😀 Platelet aggregation is a key step in clot formation, which can be disrupted by antiplatelet drugs such as Aspirin, ADP receptor blockers, and glycoprotein 2b/3a inhibitors.
- 😀 Aspirin works by irreversibly inhibiting COX-1 enzyme, disrupting thromboxane A2 production and preventing platelet activation and aggregation.
- 😀 ADP receptor inhibitors like Clopidogrel and Ticagrelor block P2Y12 receptors, preventing the activation of glycoprotein 2b/3a receptors and inhibiting platelet aggregation.
- 😀 Glycoprotein 2b/3a inhibitors (e.g., Abciximab) block the receptors that allow platelets to bind fibrinogen, preventing platelet aggregation.
- 😀 Phosphodiesterase inhibitors like Cilostazol increase cyclic AMP levels, reducing platelet activation and promoting vasodilation.
- 😀 Heparin and low-molecular-weight Heparins accelerate antithrombin activity, inactivating factor 10a and thrombin, reducing clot formation.
- 😀 Direct factor 10a inhibitors (e.g., Apixaban, Rivaroxaban) bind directly to factor 10a, preventing thrombin generation and clot formation. They are available orally.
- 😀 Direct thrombin inhibitors (e.g., Dabigatran) work by directly binding to thrombin, preventing clot formation without binding to platelet factor-4, making them suitable for Heparin-induced thrombocytopenia (HIT).
- 😀 Warfarin inhibits vitamin K epoxide reductase, preventing the synthesis of active clotting factors, requiring close INR monitoring to manage bleeding risk and drug-food interactions.
- 😀 Thrombolytics like Alteplase, Streptokinase, and Urokinase dissolve existing clots by activating plasminogen to plasmin, though they carry a risk of bleeding, particularly with less selective agents.
Q & A
What is the primary use of anticoagulants and antiplatelet agents?
-Anticoagulants and antiplatelet agents are primarily used to treat thrombotic disorders, which involve unwanted blood clots inside blood vessels that can lead to heart attacks or strokes.
How do endothelial cells normally prevent clot formation?
-In the absence of injury, endothelial cells release chemical mediators like nitric oxide, which dilates blood vessels, and prostacyclin, which binds to platelet receptors to prevent platelet activation and aggregation.
What happens when a blood vessel is damaged?
-When a blood vessel is damaged, there is a reduction in nitric oxide and prostacyclin, leading to vessel constriction and platelet activation. Platelets adhere to collagen and release granules that attract more platelets to form a plug.
What is the mechanism of action of Aspirin as an antiplatelet agent?
-Aspirin irreversibly inactivates the cyclooxygenase-1 (Cox-1) enzyme in platelets, preventing the production of thromboxane A2, a key mediator in platelet aggregation.
How do P2Y12 inhibitors, such as Clopidogrel and Ticagrelor, work to inhibit clot formation?
-P2Y12 inhibitors block the ADP receptor (specifically the P2Y12 subtype) on platelets, preventing activation of the glycoprotein 2b/3a receptors, which are necessary for fibrin-mediated platelet aggregation.
What is the role of glycoprotein 2b/3a receptor inhibitors like Abciximab and Eptifibatide?
-Glycoprotein 2b/3a receptor inhibitors bind directly to these receptors on platelets, preventing fibrinogen from binding and cross-linking platelets, thus inhibiting platelet aggregation.
What is the mechanism of action of phosphodiesterase inhibitors like Dipyridamole and Cilostazol?
-Phosphodiesterase inhibitors block the enzyme phosphodiesterase, which increases intracellular cyclic AMP levels. This leads to reduced intracellular calcium and inhibits platelet activation. Cilostazol also promotes vasodilation in peripheral arteries.
What is the role of Heparin in anticoagulation therapy?
-Heparin binds to antithrombin 3, accelerating its activity to inactivate clotting factors, particularly factor 10a and thrombin, thereby preventing clot formation.
What is Heparin-induced thrombocytopenia (HIT), and why is it a concern?
-HIT is a condition where antibodies form against Heparin-bound platelet factor-4, causing platelet activation and an increased risk of clot formation, despite low platelet counts.
How do direct oral anticoagulants like Apixaban and Rivaroxaban work?
-Apixaban and Rivaroxaban are direct inhibitors of factor 10a. By binding directly to the active site of factor 10a, they prevent the conversion of prothrombin to thrombin, thereby inhibiting clot formation.
What is the unique mechanism of action of Warfarin?
-Warfarin inhibits the enzyme vitamin K epoxide reductase, which disrupts the recycling of vitamin K, thereby preventing the synthesis of biologically active clotting factors 2, 7, 9, and 10.
How do thrombolytic agents like Alteplase and Streptokinase work?
-Thrombolytics activate plasminogen, converting it into plasmin. Plasmin then breaks down fibrin in blood clots, dissolving the clot. Agents like Alteplase are more selective for fibrin-bound plasminogen, while others like Streptokinase are less selective and may cause more bleeding.
What is the role of Protamine sulfate in anticoagulant therapy?
-Protamine sulfate is used to reverse the effects of Heparin and low-molecular-weight Heparins by binding to these agents and forming an inactive complex, thus stopping anticoagulation.
What is a significant side effect common to all antiplatelet drugs?
-The major side effect of all antiplatelet drugs is bleeding, which can lead to significant complications.
What is the advantage of using direct thrombin inhibitors over Heparin?
-Direct thrombin inhibitors, like Argatroban and Dabigatran, do not bind to platelet factor-4, making them useful in patients with Heparin-induced thrombocytopenia, and they have a more predictable anticoagulant effect compared to Heparin.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Pharmacology – ANTIBIOTICS – CELL WALL & MEMBRANE INHIBITORS (MADE EASY)
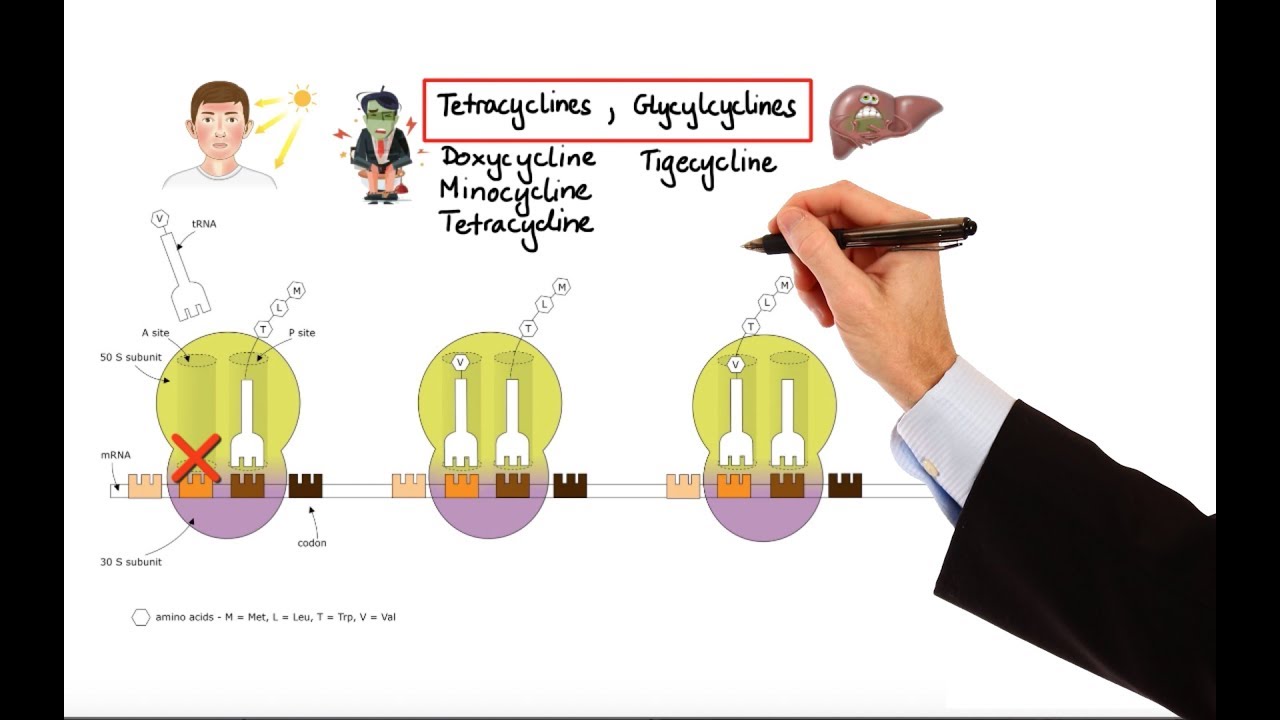
Pharmacology – ANTIBIOTICS – DNA, RNA, FOLIC ACID, PROTEIN SYNTHESIS INHIBITORS (MADE EASY)

FARMAKOLOGI ANTIHISTAMIN
GENERAL ANESTHETICS| Pharmacology| CNS| #osmosis #Mednex| 1st video
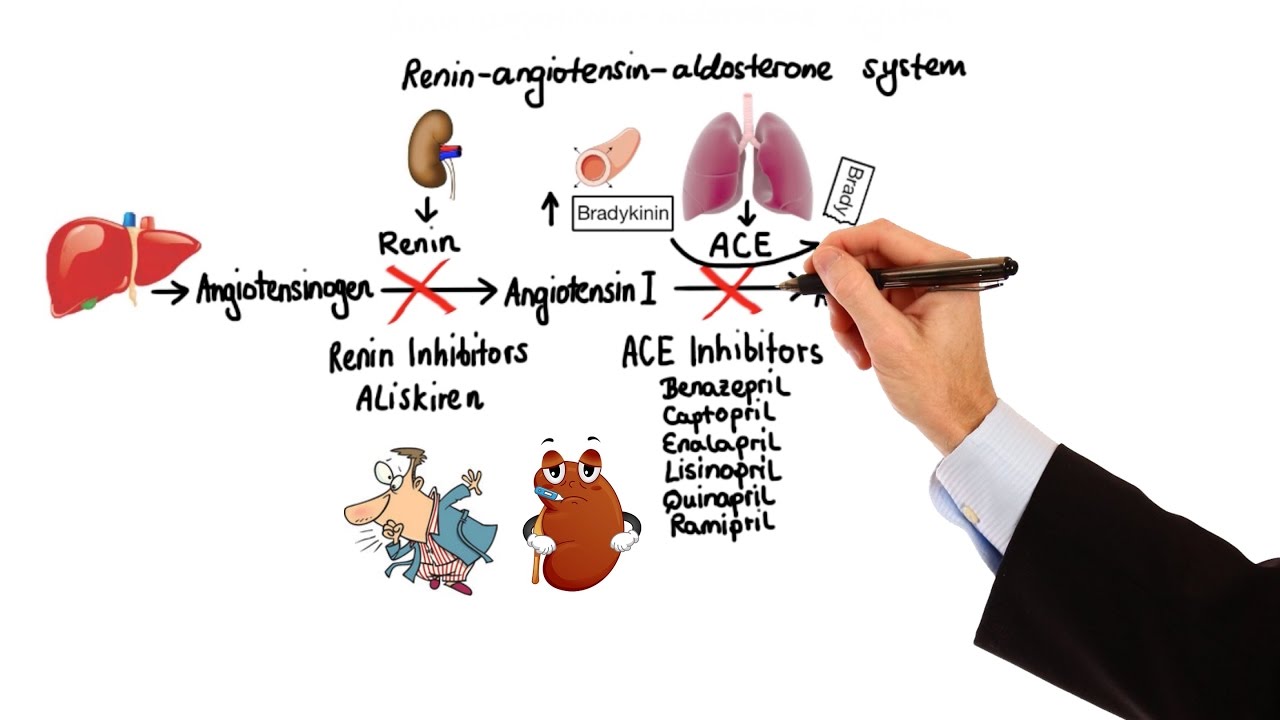
Pharmacology - HYPERTENSION & ANTIHYPERTENSIVES (MADE EASY)

Pharmacology: Oral Hypoglycemic Drugs, Animation
5.0 / 5 (0 votes)