THE INFLAMMATORY RESPONSE
Summary
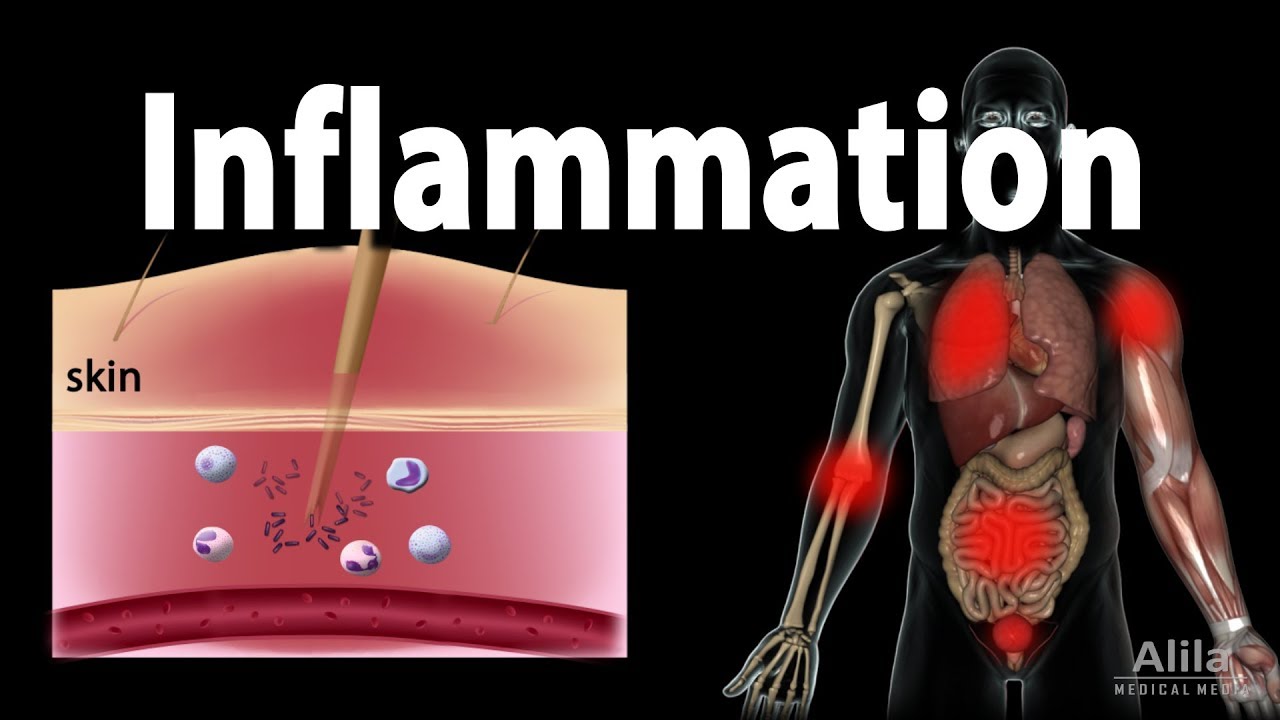
TLDRThe inflammatory response is a crucial biological process initiated by infection or injury, characterized by swelling, redness, heat, and pain. It involves four key changes in blood vessels: increased diameter, heightened permeability, activated endothelial cells, and clotting to prevent pathogen spread. Triggered by tissue damage and pathogen recognition, inflammatory mediators like cytokines and chemokines play significant roles in recruiting leukocytes to the site of infection. Neutrophils are the first responders, followed by monocytes and other leukocytes, ensuring the body can effectively combat invaders and promote tissue repair.
Takeaways
- 😀 The inflammatory response starts quickly after infection or injury, marked by heat, redness, swelling, and pain.
- 🔥 Increased vascular diameter during inflammation leads to heat and redness, while also slowing blood flow.
- 💧 Enhanced vascular permeability allows fluid and plasma proteins to leak into tissues, causing edema and pain.
- 🦠 Activated endothelial cells express adhesion molecules, facilitating the binding and migration of leukocytes to the site of infection.
- 🚧 The inflammatory response serves three main purposes: defending against pathogens, inducing local blood clotting, and promoting tissue repair.
- ⚡ Tissue damage and pathogen recognition by macrophages trigger the inflammatory response through the release of inflammatory mediators.
- 🔬 Important cytokines like C5a and TNF-α play crucial roles in attracting and activating leukocytes during inflammation.
- 🧫 Neutrophils are the first leukocytes to respond, followed by monocytes that become macrophages; later stages involve eosinophils and lymphocytes.
- 📉 Slower blood flow in inflamed tissues allows for more effective leukocyte interaction with endothelial cells.
- 🔄 Injury activates the kinin and coagulation cascades, leading to increased permeability and clot formation to contain the infection.
Q & A
What are the four main characteristics of the inflammatory response?
-The four main characteristics of the inflammatory response are edema (swelling), heat, redness, and pain at the site of infection or injury.
What causes the heat and redness associated with inflammation?
-The heat and redness are caused by an increase in vascular diameter, which also leads to slower blood flow in the affected area.
How does vascular permeability change during inflammation?
-During inflammation, the endothelial cells of blood vessel walls become more permeable due to the formation of gaps between them, allowing fluid and plasma proteins to exit into local tissues, resulting in edema.
What role do leukocytes play in the inflammatory response?
-Leukocytes, or white blood cells, are essential for attacking pathogens. They attach to activated endothelial cells and migrate into tissues through a process called extravasation.
What triggers the release of inflammatory mediators?
-Inflammatory mediators are released when tissues are physically damaged or when pathogens are recognized by macrophages, leading to an inflammatory response.
What are chemokines, and how do they function?
-Chemokines are a type of cytokine that act as chemoattractants, directing the movement of phagocytes towards their source, which is crucial for targeting areas of infection or injury.
What is the significance of C5a in the inflammatory response?
-C5a is a complement fragment that stimulates oxidative burst in phagocytes, attracts neutrophils and monocytes, increases vascular permeability, and activates mast cells to release histamine.
How does TNF-α contribute to inflammation?
-TNF-α is produced by macrophages and acts as a potent activator of endothelial cells, promoting the expression of adhesion molecules essential for leukocyte recruitment.
What are the roles of the kinin and coagulation cascades during inflammation?
-The kinin cascade produces inflammatory mediators like bradykinin, which increases vascular permeability and causes pain, while the coagulation cascade leads to the formation of a fibrin clot, preventing pathogen spread.
What types of leukocytes are involved in different stages of inflammation?
-Initially, neutrophils cross the blood vessel wall to enter inflamed tissue, followed by monocytes that differentiate into macrophages. Later stages may involve eosinophils and lymphocytes as well.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade Now5.0 / 5 (0 votes)