PPN vs. TPN (SUMMARY)
Summary
TLDRThe video discusses two main forms of parenteral nutrition: Peripheral Parenteral Nutrition (PPN) and Central Parenteral Nutrition (CPN). The primary difference lies in the type of vascular access used. PPN is delivered through a small vein in the arm or hand, suitable for short-term use, while CPN is administered through a larger vein near the heart for long-term nutrition. CPN is preferred for its ability to meet higher nutritional demands and lower risk of complications like phlebitis. PPN can serve as a temporary bridge to CPN if long-term nutrition is needed.
Takeaways
- 💉 Peripheral Parenteral Nutrition (PPN) and Central Parenteral Nutrition (CPN) are the two main types of parenteral nutrition treatments.
- 🩺 The major difference between PPN and CPN is the type of vascular access device used for nutrient delivery.
- 💪 PPN is infused into a small vein, typically in the forearm or back of the hand, while CPN is infused into a large vein near the heart.
- ⏳ PPN is recommended for short-term use (less than two weeks), whereas CPN is for longer durations (more than two weeks).
- 🔄 PPN can serve as a temporary bridge to CPN when the duration of parenteral nutrition is initially uncertain.
- ⚠️ Peripheral catheters are more prone to complications like phlebitis and extravasation, while central catheters are more durable and easier to maintain.
- 📉 PPN solutions should not exceed an osmolarity of 900 mOsm/L due to the limitations of peripheral veins.
- 🔬 CPN allows for higher osmolarity solutions, even greater than 1000 mOsm/L, because the large veins can handle rapid dilution.
- 💧 Meeting nutritional demands with PPN can be challenging, especially in patients with high nutrient needs or fluid restrictions.
- 🏥 CPN is generally the more desirable option for most patient populations due to its ability to deliver high nutrient concentrations with lower risks of complications.
Q & A
What are the two major forms of parenteral nutrition discussed in the video?
-The two major forms of parenteral nutrition discussed are peripheral parenteral nutrition (PPN) and central parenteral nutrition (CPN).
What is the main difference between PPN and CPN?
-The main difference between PPN and CPN is the type of vascular access device used. PPN is infused into a small vein, typically in the forearm or hand, while CPN is infused into a large vein, with the end position near the heart in the distal third of the superior vena cava.
Why is PPN generally recommended for short-term infusions?
-PPN is recommended for infusions lasting less than two weeks because peripheral catheters are easier to dislodge, more difficult to maintain, and are prone to complications over extended periods.
Why is CPN preferred for long-term infusions?
-CPN is preferred for long-term infusions (more than two weeks) because central catheters are more durable, easier to maintain for extended periods, and they bypass the osmolarity limitations of peripheral veins.
What is the maximum osmolarity a peripheral vein can tolerate, and why is this important?
-A peripheral vein can tolerate an osmolarity of approximately 900 milliosmoles per liter. This limitation is important because it restricts the concentration of nutrients that can be delivered via PPN, making it harder to meet a patient's nutritional needs, especially if they have fluid restrictions or high nutrient requirements.
What complications are more common with peripheral catheters in PPN?
-Complications like parenteral nutrition-induced phlebitis and extravasation are more common with peripheral catheters used in PPN.
How does CPN overcome the osmolarity limitations faced by PPN?
-CPN overcomes osmolarity limitations by using a large vein with high blood flow, which rapidly dilutes the parenteral nutrition solution, allowing for higher osmolarity (greater than 1000 milliosmoles per liter) without complications.
When might a patient transition from PPN to CPN?
-A patient might transition from PPN to CPN if the duration of parenteral nutrition becomes longer than initially expected. PPN can be used as a bridge to CPN when the need for nutrition exceeds two weeks.
Why is it difficult to meet high nutrient needs with PPN, especially in fluid-restricted patients?
-It is difficult to meet high nutrient needs with PPN because of the osmolarity limit of 900 milliosmoles per liter, which restricts the concentration of nutrients like dextrose, amino acids, and electrolytes. This becomes especially challenging in fluid-restricted patients where the volume of the solution must be kept low.
What makes CPN the more desirable option across a wide range of patient populations?
-CPN is more desirable because it allows for the delivery of a higher concentration of nutrients in a small volume, is less prone to complications like phlebitis and extravasation, and is better suited for meeting the nutritional demands of a wide range of patients, including those requiring long-term care.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video
How to Design Total Parenteral Nutrition

When to Use Parenteral Nutrition

Administering Parenteral Nutrition Through a Central Line

Nutrition Therapy Overview: Specialty Diets, Administration Methods & Benefits | Lecturio Nursing

11 Nutrition Care Plan for Terminally Ill or Hospice Patient
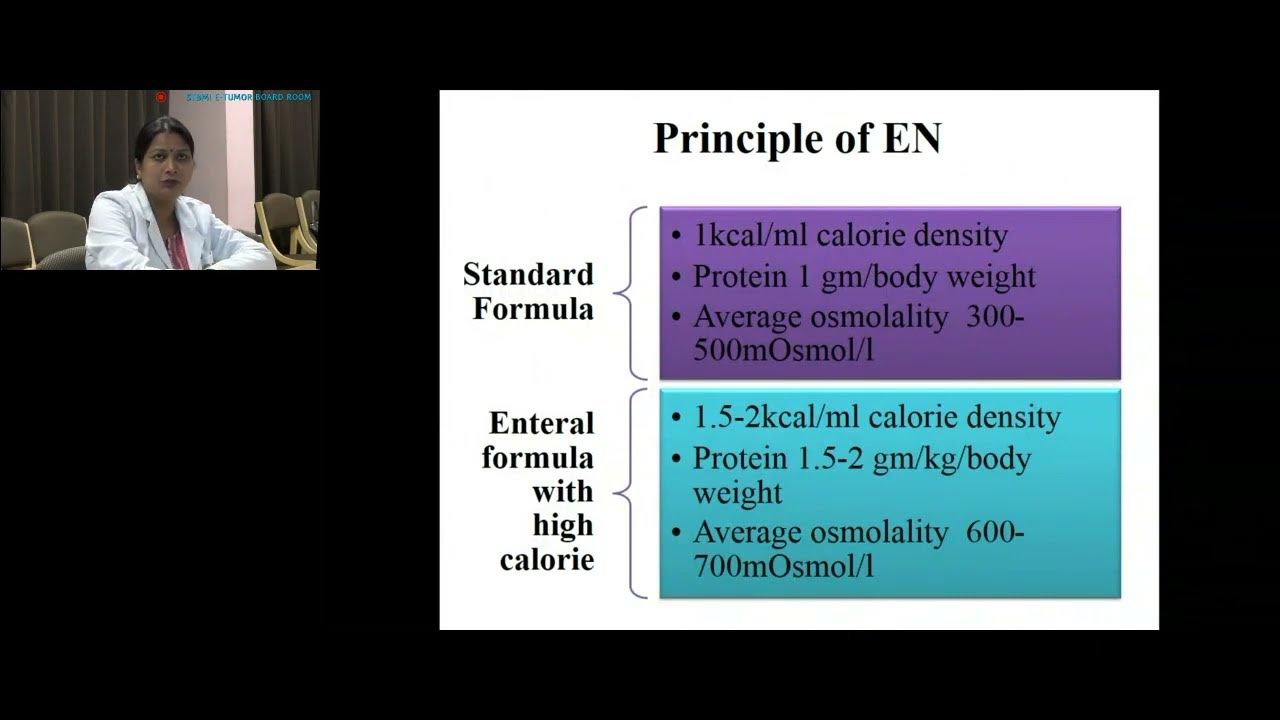
Nutrition in ICU by Shilpi Pandey, SGPGIMS, Lucknow
5.0 / 5 (0 votes)