Liver Function Tests - an overview
Summary
TLDRThis educational video by Dr. Matt delves into liver function tests, explaining what they are and their purpose. It covers key enzymes like AST, ALT, ALP, and GGT, and liver-produced substances like albumin, prothrombin time, and bilirubin. The video discusses why these tests might be ordered, such as for patients with liver disease, medication-induced liver injury, or high-risk groups. It also provides a schematic approach to interpreting test results, distinguishing between jaundice causes, cholestasis, and hepatocellular injury, offering valuable insights for medical professionals.
Takeaways
- 🧬 Liver function tests (LFTs) are blood biomarkers that indicate liver health, including enzymes and liver-produced products like albumin and bilirubin.
- 🔬 Enzymes such as AST (Aspartate Transaminase), ALT (Alanine Transaminase), ALP (Alkaline Phosphatase), and GGT (Gamma Glutamyl Transferase) are released by the liver and can signal liver injury if elevated.
- 📈 Albumin, prothrombin time, and bilirubin levels are liver-produced substances that, when abnormal, suggest liver dysfunction in protein synthesis, clotting factor production, and bilirubin processing, respectively.
- 🏥 LFTs may be ordered to investigate liver disease, medication or poison-induced liver injury, alcohol use, family history of liver issues, or high-risk groups such as those exposed to viral hepatitis or illicit drugs.
- 🔎 Jaundice, a yellow discoloration of skin and eyes due to bilirubin buildup, can be assessed through LFTs to determine its cause, such as pre-hepatic, intra-hepatic, or post-hepatic conditions.
- 📊 Bilirubin levels above 1.2 mg/dL may indicate jaundice and require further investigation into the cause, which could be related to red blood cell breakdown or liver processing issues.
- 🚫 High levels of ALP and GGT in conjunction suggest cholestasis, a blockage in bile flow, but must be differentiated from non-liver sources like bone tissue.
- ⚕️ AST and ALT are key indicators of hepatocellular injury; their levels and ratio can help differentiate between acute and chronic liver conditions, with AST being more sensitive to alcohol.
- 📉 Decreased albumin and clotting factors, along with increased clotting time, indicate liver's compromised ability to produce necessary proteins and regulate blood clotting.
- 🛑 Hepatocellular injury affects bilirubin processing, leading to issues in secretion and excretion, and can result in both pre-hepatic and post-hepatic jaundice.
- 🧐 Understanding the nuances of LFTs, such as the role of individual enzymes and liver-produced substances, is crucial for diagnosing and managing liver conditions.
Q & A
What are liver function tests, and what do they measure?
-Liver function tests, also known as liver chemistries, are blood biomarkers that indicate how well the liver is functioning. They measure the levels of certain enzymes and proteins that are either produced by the liver or are indicative of liver function, such as AST, ALT, ALP, GGT, albumin, prothrombin time, and bilirubin.
What is the significance of enzymes like AST and ALT in liver function tests?
-AST (Aspartate Transaminase) and ALT (Alanine Transaminase) are enzymes that are released from the liver. Elevated levels of these enzymes can indicate liver injury or disease, as they are markers of hepatocellular damage.
What are the liver-produced products that liver function tests measure?
-The liver-produced products measured by liver function tests include albumin, a protein that helps maintain blood volume and pressure; prothrombin time, which reflects the liver's ability to produce clotting factors; and bilirubin, which is processed and conjugated by the liver for excretion.
Why might a healthcare provider order liver function tests?
-Liver function tests may be ordered to investigate potential liver issues, such as a history of liver disease, exposure to hepatotoxic medications, alcohol use, or a family history of liver disorders. They can also be used as a screening tool for high-risk patients or to monitor liver function in patients with conditions that may affect the liver.
What is jaundice, and how can liver function tests help diagnose its cause?
-Jaundice is a yellow discoloration of the skin and eyes due to a buildup of bilirubin. Liver function tests can help determine the cause of jaundice by measuring the levels of bilirubin and other liver enzymes, which can indicate whether the issue is pre-hepatic, hepatic, or post-hepatic.
How does the liver process bilirubin, and why is it important?
-The liver processes bilirubin by conjugating it, making it water-soluble and allowing it to be excreted via bile. This process is crucial for the elimination of bilirubin from the body and helps maintain normal bilirubin levels, which is important for overall health.
What is the difference between pre-hepatic, intra-hepatic, and post-hepatic causes of jaundice?
-Pre-hepatic causes of jaundice are related to increased red blood cell destruction or issues with the enzyme that conjugates bilirubin. Intra-hepatic causes involve problems within the liver cells, such as diseases affecting liver function. Post-hepatic causes are related to obstructions in bile flow, such as blockages in the bile ducts.
How can the ratio of direct to total bilirubin help determine the cause of jaundice?
-A higher proportion of direct bilirubin compared to total bilirubin can suggest a post-hepatic cause of jaundice, such as cholestasis, where there is a problem with bile excretion. Conversely, a higher total bilirubin compared to direct bilirubin may indicate a pre-hepatic cause, such as increased red blood cell destruction or issues with bilirubin conjugation.
What role do bile acids play in the diagnosis of cholestasis through liver function tests?
-In cholestasis, bile acids can accumulate and cause an increase in the activity of enzymes such as alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT), which are found on the bile canalicular membrane of hepatocytes. Elevated levels of these enzymes can indicate a problem with bile excretion.
How can the levels of AST and ALT help differentiate between acute and chronic liver injury?
-Significantly elevated levels of AST and ALT, such as 10 times the normal value, can indicate acute liver injury, which could be due to factors like viral hepatitis, drug toxicity, or hypoxic injury. Moderate increases in these enzymes, around five times the normal value, may suggest chronic liver injury, possibly due to conditions like fatty liver disease or chronic viral hepatitis.
Why might the ratio of AST to ALT be higher in cases of alcohol-induced liver injury?
-The higher ratio of AST to ALT in cases of alcohol-induced liver injury is due to the fact that AST is more sensitive to alcohol's effects on the mitochondria, which can cause it to leak into the bloodstream at a higher rate than ALT. Additionally, chronic liver conditions like cirrhosis can also lead to a higher AST to ALT ratio.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Field Study 1-Learning Episode 1: The School Environment
Should Letter Grades Be Abandoned?
Chemistry Lesson: Molecular, Complete Ionic & Net Ionic Equations

What are Trace Fossils? | A New Way to Museum

Plato, Crito | Crito's Arguments with Socrates | Philosophy Core Concepts

Japan's Education System
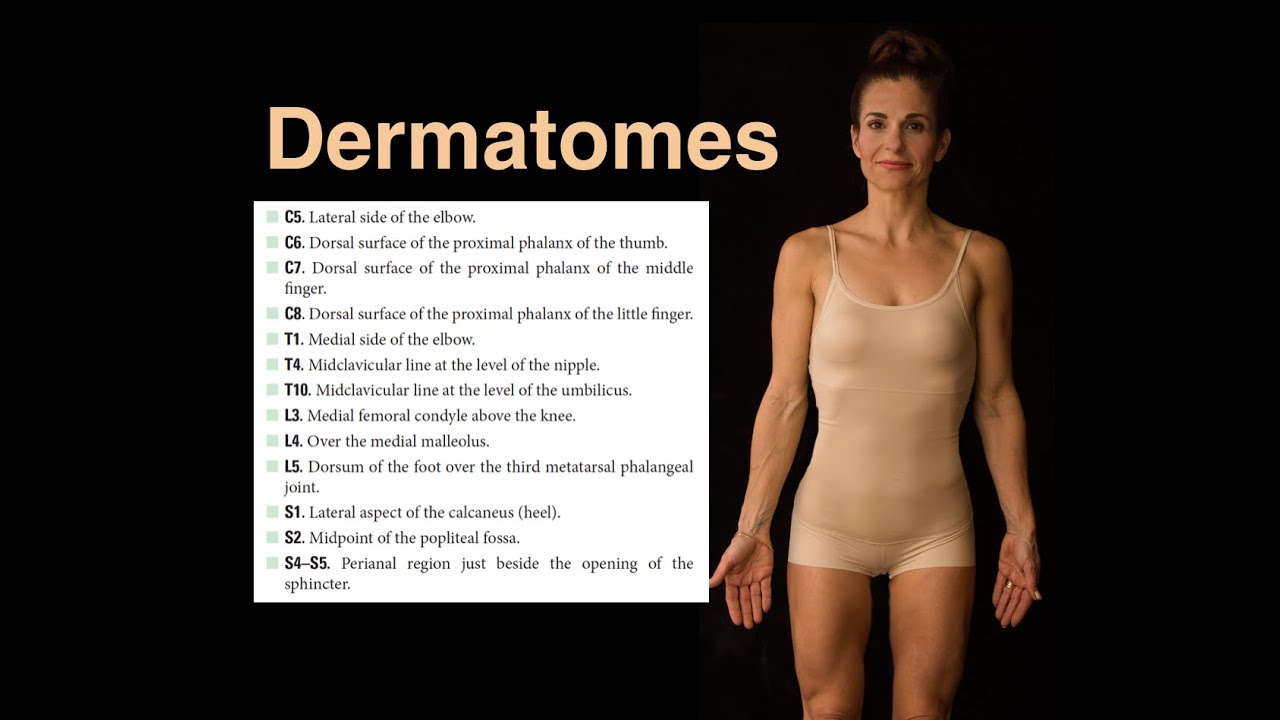
Dermatomes
5.0 / 5 (0 votes)