Hipersensibilidade Tipo IV. Hipersensibilidade Tipo Tardio (Mediada por Linfócitos T)
Summary
TLDRThis video discusses the role of T cells in autoimmune diseases, focusing on type 1 diabetes, rheumatoid arthritis, multiple sclerosis, psoriasis, and inflammatory bowel disease. It explains how Th1 and CD8 T cells contribute to tissue destruction by releasing inflammatory cytokines and activating immune responses. In type 1 diabetes, for example, T cells destroy pancreatic beta cells, leading to insulin production failure. The video also explores the complexity of these diseases, the involvement of autoantibodies, and how targeting these pathways could lead to better treatments.
Takeaways
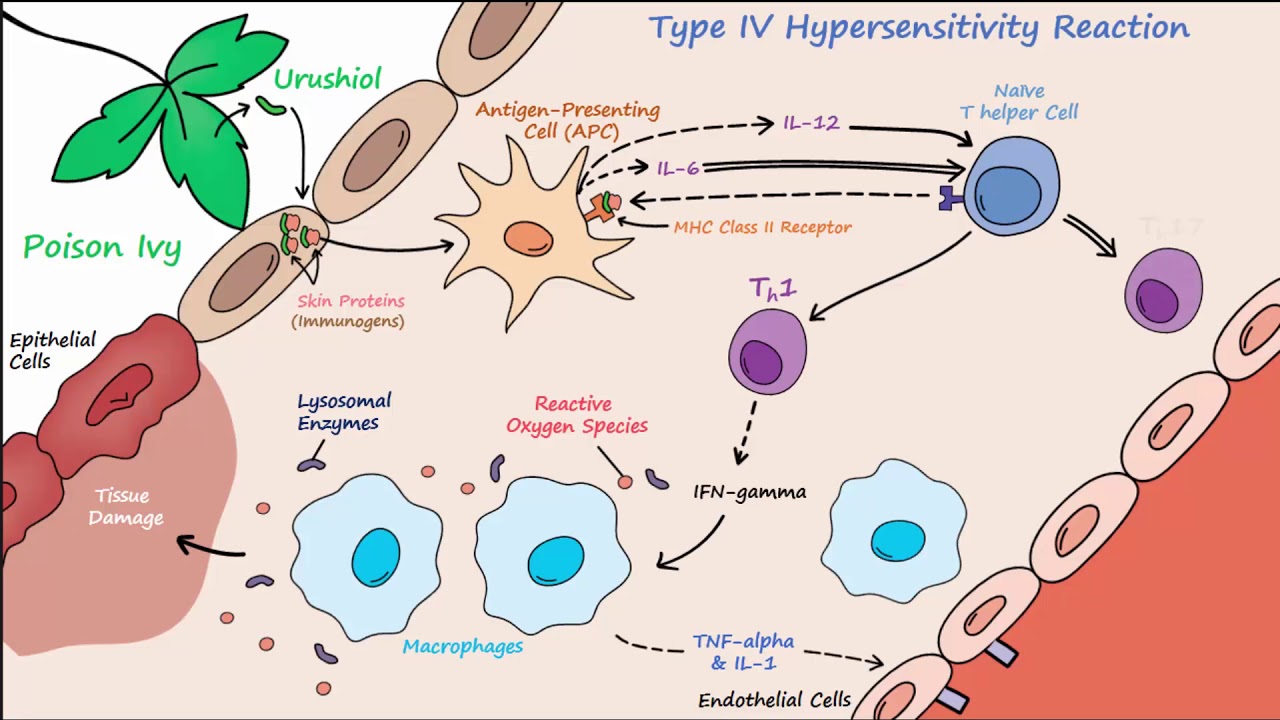
- 😀 Type 4 hypersensitivity is mediated by T cells, leading to inflammation and tissue damage.
- 😀 In type 1 diabetes, Th1 cells and CD8 T cells contribute to the destruction of pancreatic beta cells, leading to insulin deficiency.
- 😀 Autoantibodies play a role in type 1 diabetes by binding to pancreas tissues, triggering macrophages and neutrophils to further damage the pancreas.
- 😀 The complement system is activated in type 1 diabetes, amplifying tissue destruction and inflammation in the pancreas.
- 😀 Rheumatoid arthritis involves T cells, particularly Th1 and Th17 cells, which contribute to inflammation through cytokine release and immune complexes.
- 😀 Multiple sclerosis is characterized by T cells targeting myelin proteins, resulting in myelin destruction by activated macrophages.
- 😀 Psoriasis, particularly guttate psoriasis, may be triggered by recurrent tonsil infections, with a cross-reaction involving skin proteins and bacterial proteins.
- 😀 Inflammatory bowel disease (IBD) is associated with T cells targeting enteric bacteria and self-antigens, with inflammation mediated by Th17 cells.
- 😀 Type 1 diabetes is a form of childhood diabetes where T cells target pancreatic islet antigens like glutamic acid decarboxylase, leading to insulin production failure.
- 😀 The presence of Th1 cells, CD8 T cells, and autoantibodies makes autoimmune diseases complex, requiring targeted therapeutic interventions to alter the immune response.
Q & A
What is the role of Th1 cells in autoimmune diseases like Type 1 Diabetes?
-Th1 cells release cytokines that increase the inflammatory response in the pancreas, leading to the recruitment of leukocytes and further tissue damage. In Type 1 Diabetes, this results in the destruction of pancreatic beta cells, impairing insulin production.
How do CD8 T cells contribute to the destruction of pancreatic beta cells in Type 1 Diabetes?
-CD8 T cells, also known as cytotoxic T lymphocytes, release granzymes that directly target and destroy pancreatic beta cells, leading to a loss of insulin production.
What is the role of autoantibodies in the destruction of pancreatic tissue in autoimmune diseases?
-Autoantibodies bind to specific tissue sites, such as in the pancreas, triggering the degranulation of macrophages and neutrophils. This leads to further tissue damage through phagocytosis and inflammatory responses.
What other immune system components are involved in the destruction of pancreatic beta cells in Type 1 Diabetes?
-In addition to Th1 and CD8 T cells, the complement system and B cells also play roles. B cells produce autoantibodies, while the complement system contributes to the inflammation and tissue damage.
What is the significance of the M protein in the development of guttate psoriasis?
-The M protein, produced during recurrent palatine tonsil infections, mimics skin proteins, which leads to a cross-reaction that triggers guttate psoriasis in individuals with repeated tonsil infections.
Why do some individuals with guttate psoriasis experience improvement after tonsil removal?
-Guttate psoriasis is linked to recurrent palatine tonsil infections. Removing the tonsils reduces the trigger for the cross-reaction caused by the M protein, leading to significant improvement in psoriasis symptoms.
What is the role of Th17 cells in diseases like psoriasis and rheumatoid arthritis?
-Th17 cells play a central role in the inflammatory processes of psoriasis and rheumatoid arthritis, releasing cytokines that promote tissue damage and inflammation. In psoriasis, they cause skin inflammation, while in rheumatoid arthritis, they contribute to joint inflammation.
What is the main pathogenic mechanism in multiple sclerosis?
-In multiple sclerosis, T cells target proteins in the myelin sheath of neurons. This leads to inflammation and the destruction of myelin by activated macrophages, impairing nerve function.
What is the current understanding of the role of T-cells in inflammatory bowel disease (IBD)?
-The exact cause of IBD is still not fully understood, but T-cells are thought to contribute by targeting both enteric bacteria and self-antigens, leading to chronic inflammation in the intestines.
How does the immune response differ in Type 1 and Type 2 diabetes?
-Type 1 Diabetes is an autoimmune disease where the immune system attacks pancreatic beta cells, impairing insulin production. Type 2 Diabetes, on the other hand, is typically caused by insulin resistance and is not mediated by an autoimmune process.
Outlines

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードMindmap

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードKeywords

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードHighlights

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードTranscripts

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレード関連動画をさらに表示
Type IV Hypersensitivity (Described Concisely)

Type IV Hypersensitivity |T- Cell mediated Hypersensitivity |Mechanism | Examples

Hipersensibilidades (Parte II - Hipersensibilidades dos tipos II, III e IV)

gangguan pada sistem imun/ sistem pertahanan tubuh - biologi sma kelas 11 semester 2 bab.sistem imun

Yang Lagi Pegel-Pegel, Nonton Ini!

When Your Body Attacks Itself – Autoimmune
5.0 / 5 (0 votes)
