BiPAP vs CPAP (Made Easy) | Noninvasive Positive Pressure Ventilation (NPPV)
Summary
TLDRThis video explains the key differences between BiPAP and CPAP, two types of non-invasive positive pressure ventilation. Non-invasive ventilation aims to prevent intubation and reduce complications associated with mechanical ventilation. CPAP delivers continuous pressure throughout the breathing cycle, mainly used for obstructive sleep apnea, while BiPAP offers two pressure levels to assist with conditions like acute respiratory failure and COPD exacerbations. The video also discusses indications, contraindications, patient interfaces, and titration of settings, providing a comprehensive understanding of when to use each therapy effectively.
Takeaways
- 😀 Non-invasive ventilation aims to provide positive pressure ventilation without an artificial airway, reducing complications associated with intubation.
- 😀 The two main types of non-invasive ventilation are BiPAP (Bi-level Positive Airway Pressure) and CPAP (Continuous Positive Airway Pressure).
- 😀 CPAP delivers a constant pressure throughout the breathing cycle and is primarily indicated for obstructive sleep apnea.
- 😀 BiPAP provides two levels of pressure: IPAP during inhalation and EPAP during exhalation, making it suitable for conditions like acute respiratory failure.
- 😀 Common indications for non-invasive ventilation include severe dyspnea, acute exacerbation of COPD, and congestive heart failure.
- 😀 CPAP is contraindicated in patients who are apneic, hypoventilating, or experiencing respiratory muscle fatigue.
- 😀 Interfaces used for CPAP and BiPAP include nasal masks, oral-nasal masks, nasal pillows, and full face masks, each with specific advantages and potential issues.
- 😀 Proper titration of non-invasive ventilation settings is crucial, with common starting pressures around 10 cm H2O for IPAP and 5 cm H2O for EPAP.
- 😀 Monitoring patients on CPAP is essential to detect signs of fatigue, such as increased respiratory rate or accessory muscle use.
- 😀 Both BiPAP and CPAP have contraindications, including facial burns/trauma and claustrophobia, which must be considered before use.
Q & A
What is non-invasive positive pressure ventilation?
-Non-invasive positive pressure ventilation is a method of providing positive pressure ventilation without using an artificial airway, aiming to avoid intubation and reduce complications associated with traditional mechanical ventilation.
What are the two primary types of non-invasive ventilation covered in the video?
-The two primary types of non-invasive ventilation discussed are BiPAP (Bi-level Positive Airway Pressure) and CPAP (Continuous Positive Airway Pressure).
What does the acronym CPAP stand for, and how does it function?
-CPAP stands for Continuous Positive Airway Pressure, which delivers and maintains positive pressure throughout the entire breathing cycle, but only when the patient is breathing spontaneously.
What are the primary settings for non-invasive ventilation?
-The primary settings for non-invasive ventilation are Ipap (Inspiratory Positive Airway Pressure) and Epap (Expiratory Positive Airway Pressure). Ipap influences the tidal volume, while Epap improves oxygenation by increasing functional residual capacity.
What conditions are common indications for using non-invasive ventilation?
-Common indications for non-invasive ventilation include severe dyspnea, acute respiratory failure, acute exacerbation of COPD, congestive heart failure, pulmonary edema, and obstructive sleep apnea.
What are some contraindications for using CPAP?
-Contraindications for CPAP include apnea and hypoventilation, respiratory muscle fatigue, facial burns or trauma, and claustrophobia.
How does BiPAP differ from CPAP?
-BiPAP delivers two levels of pressure (Ipap and Epap), while CPAP delivers a continuous single pressure throughout the breathing cycle. This allows BiPAP to better manage ventilatory issues.
What is a common starting point for the settings in non-invasive positive pressure ventilation?
-A common starting point for non-invasive positive pressure ventilation is 10 over 5, meaning an Ipap setting of 10 cm H2O and an Epap setting of 5 cm H2O.
What types of masks are used for BiPAP and CPAP therapies?
-Common interfaces for BiPAP and CPAP include nasal masks, oral-nasal masks, nasal pillows, and full face masks, each with specific advantages and potential complications.
What should be monitored when using CPAP?
-When using CPAP, patients should be monitored for signs of fatigue, such as dyspnea, tachycardia, increased PaCO2 levels, and decreased tidal volume, as they are providing all the minute ventilation.
Outlines

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraMindmap

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraKeywords

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraHighlights

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraTranscripts

Esta sección está disponible solo para usuarios con suscripción. Por favor, mejora tu plan para acceder a esta parte.
Mejorar ahoraVer Más Videos Relacionados

CPAP vs BiPAP - Non-Invasive Ventilation EXPLAINED

[#2] MECÂNICA RESPIRATÓRIA: PRESSÃO INTRAPLEURAL E PRESSÃO TRANSPULMONAR | MK Fisiologia

Ventilator Alarms, Modes, Settings made simple for Nursing NCLEX, RN LPN
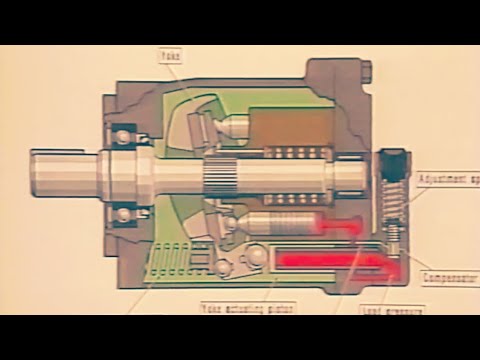
Hydraulic Training Series - Chapter 2 - Hydraulic Pumps

Basic Vent Modes MADE EASY - Ventilator Settings Reviewed

Monitorização Hemodinâmica
5.0 / 5 (0 votes)
