Congestive Heart Failure | Clinical Medicine
Summary
TLDRThis video script delves into the clinical aspects of heart failure, distinguishing between left and right heart failure and high-output failure. It discusses the pathophysiology, causes, and complications associated with each type, highlighting the importance of left ventricular ejection fraction and the role of systemic vascular resistance. The script also covers the diagnostic approach and treatment strategies, including medication therapy, device therapy, and potential transplant considerations for severe cases, aiming to reduce mortality and improve patient outcomes.
Takeaways
- 🚑 **Heart Failure Overview**: The script discusses heart failure, covering its types, pathophysiology, and clinical aspects within clinical medicine.
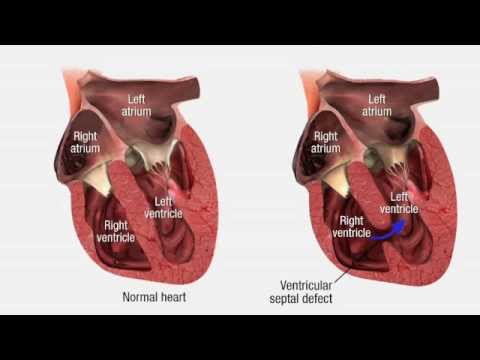
- 📈 **Pathophysiology of Heart Failure**: It differentiates between left heart failure, right heart failure, and high-output failure, detailing the pathophysiological processes behind each type.
- 🔍 **Systolic vs. Diastolic Heart Failure**: The script explains the differences between systolic heart failure (reduced contractility and ejection fraction) and diastolic heart failure (difficulty filling the heart with preserved ejection fraction).
- 💊 **Causes of Heart Failure**: It identifies common causes of heart failure, such as myocardial infarction, cardiomyopathies, and aortic stenosis, which affect the heart's ability to pump blood effectively.
- 📉 **Ejection Fraction Importance**: The left ventricular ejection fraction (LVEF) is highlighted as a critical measure, with a reduced LVEF indicating systolic heart failure (HFrEF) and a preserved LVEF indicating diastolic heart failure (HFpEF).
- 🌡️ **Compensatory Mechanisms**: The body's compensatory mechanisms, such as the renin-angiotensin-aldosterone system and sympathetic nervous system activation, are explained in response to reduced cardiac output.
- 💔 **Complications of Heart Failure**: The script outlines complications of heart failure, including pulmonary edema, cardiogenic shock, and organ malperfusion due to decreased systemic perfusion.
- 🩺 **Diagnosis of Heart Failure**: It describes the diagnostic approach to heart failure, including the use of chest X-rays, BNP levels, echocardiograms, and right heart catheterization.
- 🛠️ **Treatment Strategies**: The script covers the treatment of heart failure, emphasizing guideline-directed medical therapy, device therapy, and the use of inotropes and mechanical circulatory support in severe cases.
- 🛑 **Acute Decompensation**: It discusses the management of acute decompensated heart failure, including the use of diuretics, BiPAP, and the consideration of mechanical support such as ECMO and LVADs.
- 🏥 **Patient Management**: The importance of a systematic approach to patient management in heart failure, from risk factor modification to advanced therapies like cardiac transplantation, is emphasized.
Q & A
What is the main focus of the video script?
-The main focus of the video script is to discuss heart failure, covering its types, pathophysiology, causes, and the different aspects of left and right heart failure.
What are the two primary subtypes of left heart failure mentioned in the script?
-The two primary subtypes of left heart failure mentioned are systolic heart failure and diastolic heart failure.
What is systolic heart failure?
-Systolic heart failure occurs when there is a reduction in the contractility of the left ventricular myocardium, often caused by conditions such as myocardial infarction, dilated cardiomyopathy, or myocarditis, leading to a drop in left ventricular ejection fraction (LVEF).
What does LVEF stand for and why is it important in systolic heart failure?
-LVEF stands for Left Ventricular Ejection Fraction, which is the amount of blood pumped out of the heart with each contraction. It is important in systolic heart failure because a reduced LVEF indicates poor contractility and is used to diagnose heart failure with reduced ejection fraction (HFrEF).
What are the common causes of diastolic heart failure?
-Diastolic heart failure is commonly caused by conditions that increase afterload, such as chronic hypertension and aortic stenosis, leading to left ventricular hypertrophy and difficulty in filling the ventricle.
How does high output heart failure differ from typical heart failure?
-High output heart failure is characterized by increased cardiac output due to systemic vasodilation, which, despite the high output, is not sufficient to meet the body's oxygen demands, leading to tissue hypoperfusion.
What are the potential complications of heart failure mentioned in the script?
-The potential complications of heart failure include pulmonary congestion, pulmonary edema, cardiogenic shock, organ malperfusion, and the development of conditions such as hypoxia, acute kidney injury (AKI), and lactic acidosis.
What is the role of the renin-angiotensin-aldosterone system (RAAS) in heart failure?
-The RAAS plays a significant role in the compensatory mechanisms during heart failure. Activation of the RAAS increases systemic vascular resistance (SVR) and promotes sodium and water retention, which can worsen heart failure by increasing preload and afterload.
What are some of the treatment strategies for heart failure discussed in the script?
-Treatment strategies for heart failure include the use of medications like ACE inhibitors, ARBs, beta-blockers, diuretics, aldosterone antagonists, and sglt2 inhibitors. Other treatments involve device therapies such as CRT, ICDs, and LVADs, and in severe cases, the use of inotropes or mechanical circulatory support like ECMO.
How does the body compensate for decreased cardiac output in heart failure?
-The body compensates for decreased cardiac output by increasing systemic vascular resistance (SVR) through the activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system, which can lead to vasoconstriction and fluid retention.
What diagnostic tools are used to assess heart failure according to the script?
-Diagnostic tools used to assess heart failure include chest X-ray, B-type natriuretic peptide (BNP) levels, echocardiogram, EKG, and in more severe cases, right heart catheterization to measure pulmonary capillary wedge pressure.
Outlines

Dieser Bereich ist nur für Premium-Benutzer verfügbar. Bitte führen Sie ein Upgrade durch, um auf diesen Abschnitt zuzugreifen.
Upgrade durchführenMindmap

Dieser Bereich ist nur für Premium-Benutzer verfügbar. Bitte führen Sie ein Upgrade durch, um auf diesen Abschnitt zuzugreifen.
Upgrade durchführenKeywords

Dieser Bereich ist nur für Premium-Benutzer verfügbar. Bitte führen Sie ein Upgrade durch, um auf diesen Abschnitt zuzugreifen.
Upgrade durchführenHighlights

Dieser Bereich ist nur für Premium-Benutzer verfügbar. Bitte führen Sie ein Upgrade durch, um auf diesen Abschnitt zuzugreifen.
Upgrade durchführenTranscripts

Dieser Bereich ist nur für Premium-Benutzer verfügbar. Bitte führen Sie ein Upgrade durch, um auf diesen Abschnitt zuzugreifen.
Upgrade durchführenWeitere ähnliche Videos ansehen

Heart failure: Pathology review

Gagal Jantung (Heart Failure) - Patofisiologi CHF (Chronic Heart Failure)
Cardiovascular Pathology - Heart Disease
Left-Sided Heart Failure vs Right-Sided Heart Failure Pathophysiology Nursing NCLEX Review
CARDIOPATIA ISQUÊMICA E INSUFICIÊNCIA CARDÍACA CONGESTIVA - PATOLOGIA 28

How To Treat Heart Failure (High-Yield Guide)
5.0 / 5 (0 votes)
