Diabetic Ketoacidosis DKA Nursing | DKA Pathophysiology Treatment Management NCLEX
Summary
TLDRIn this educational video, Nurse Sarah from Nurse Orion explains diabetic ketoacidosis (DKA), a life-threatening condition common in Type 1 diabetes. She covers its pathophysiology, including the role of glucose, insulin, and ketones in the body, and discusses causes such as illness, insulin non-compliance, and missed meals. Sarah highlights the symptoms, including polyuria, dehydration, fruity breath, and tachycardia. She emphasizes key nursing interventions, such as monitoring blood glucose, administering insulin and fluids, and managing potassium levels to prevent complications like cerebral edema. The video is a vital resource for nursing students preparing for NCLEX exams.
Takeaways
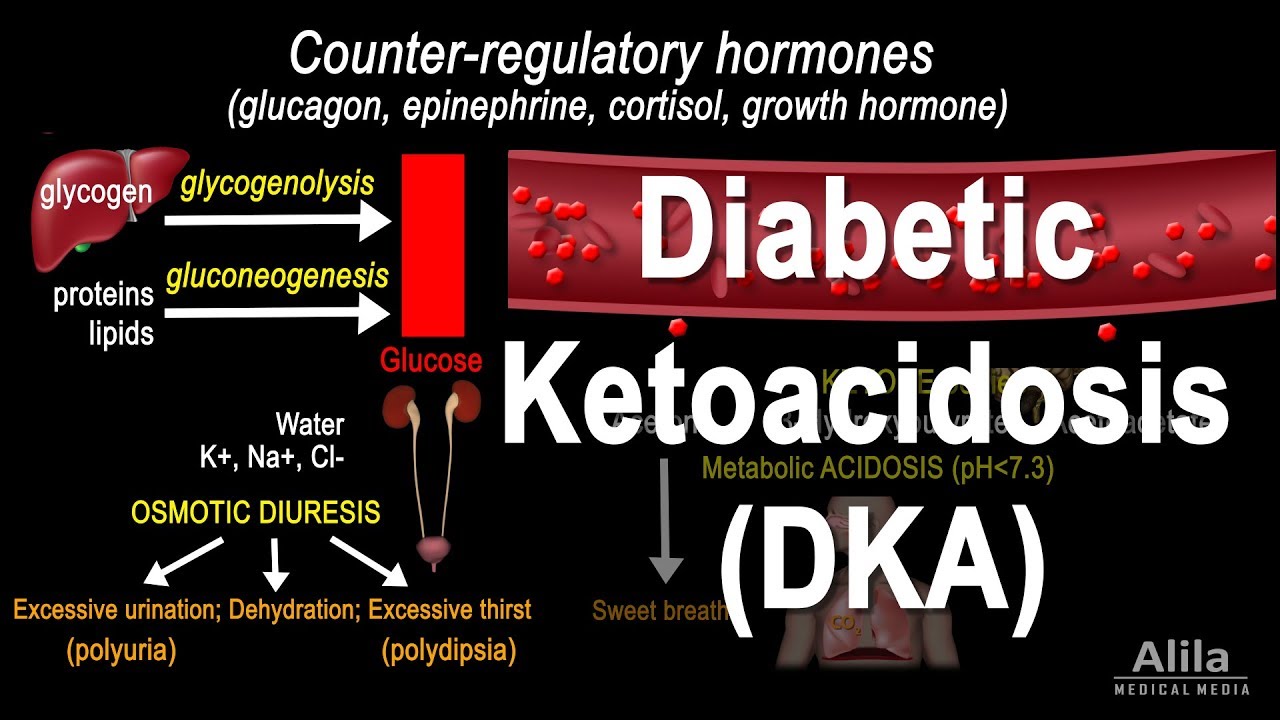
- 😀 DKA (Diabetic Ketoacidosis) is a life-threatening condition caused by insufficient insulin, leading to hyperglycemia, ketosis, and acidosis.
- 😀 The three primary factors in DKA are hyperglycemia, ketosis (ketones in the blood), and acidosis (low pH, typically < 7.35).
- 😀 Insulin's role is to move glucose into cells for energy. Without it, glucose accumulates in the blood, prompting the liver to release stored glucose, worsening the hyperglycemia.
- 😀 When the body cannot access glucose, it breaks down fats for energy, producing ketones, which are acidic and lead to metabolic acidosis.
- 😀 In DKA, the kidneys cannot reabsorb glucose, leading to osmotic diuresis (excessive urination), dehydration, and electrolyte imbalances like low sodium and potassium.
- 😀 DKA commonly occurs in Type 1 diabetes but can also occur in Type 2 under extreme stress or illness.
- 😀 Major causes of DKA include undiagnosed diabetes, illness, stress, skipping meals, or non-compliance with insulin therapy.
- 😀 Symptoms of DKA include polyuria (frequent urination), polydipsia (excessive thirst), dehydration, fruity acetone breath, nausea, vomiting, and rapid deep breathing (Kussmaul respiration).
- 😀 Nursing interventions for DKA focus on rehydration, correcting electrolyte imbalances, administering insulin (only regular insulin IV), and monitoring potassium levels to prevent hypokalemia.
- 😀 Pharmacological management includes administering IV fluids (typically normal saline), adjusting insulin drips to gradually lower blood glucose, and monitoring for signs of cerebral edema as blood sugar drops.
Q & A
What is diabetic ketoacidosis (DKA)?
-Diabetic ketoacidosis (DKA) is a life-threatening condition that occurs when there is a severe lack of insulin in the body. This leads to hyperglycemia (high blood sugar), ketosis (production of ketones from fat breakdown), and acidosis (an acidic environment in the body).
What are the three key characteristics of DKA?
-The three key characteristics of DKA are hyperglycemia (high blood sugar), ketosis (production of ketones), and acidosis (low blood pH due to ketones).
What role does insulin play in the body, and why is it absent in DKA?
-Insulin helps glucose enter cells for energy. In DKA, insulin is absent or ineffective, which prevents glucose from entering cells, leading the body to break down fats for energy instead.
How does the body compensate for the lack of glucose in DKA?
-When the body cannot access glucose due to a lack of insulin, it compensates by breaking down fats into ketones, which are then used as an alternative energy source. However, the accumulation of ketones leads to acidosis.
What happens to potassium levels in DKA, and why is it important to monitor them?
-In DKA, potassium levels are often elevated or normal because potassium moves out of cells into the bloodstream as part of the body's response to acidosis. However, when insulin is administered, potassium shifts back into cells, potentially causing hypokalemia (low potassium levels), which can be dangerous and requires careful monitoring.
What is the main cause of polyuria (frequent urination) in DKA?
-Polyuria occurs in DKA due to osmotic diuresis. The high glucose concentration in the blood draws water into the kidneys, leading to increased urination.
What are Kussmaul respirations, and why do they occur in DKA?
-Kussmaul respirations are rapid, deep breaths that occur as the body tries to compensate for metabolic acidosis by blowing off carbon dioxide, a form of acid, to help reduce the acidity in the blood.
What are the main causes of DKA?
-The main causes of DKA include undiagnosed diabetes, increased insulin needs due to illness or stress, non-compliance with insulin therapy, and skipping meals or not eating enough.
How should insulin be administered to a patient with DKA?
-Insulin should be administered intravenously, typically as a regular insulin drip. A bolus of insulin is given initially, followed by a drip that is titrated based on blood glucose levels. It's crucial to monitor potassium levels before and during insulin administration.
What are the key nursing interventions for a patient with DKA?
-Key nursing interventions include administering IV fluids (starting with normal saline), insulin, monitoring electrolytes (especially potassium), and checking for signs of cerebral edema. Nurses should also educate patients on monitoring blood glucose, urine ketones, and staying hydrated.
Outlines

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنMindmap

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنKeywords

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنHighlights

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنTranscripts

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآن5.0 / 5 (0 votes)