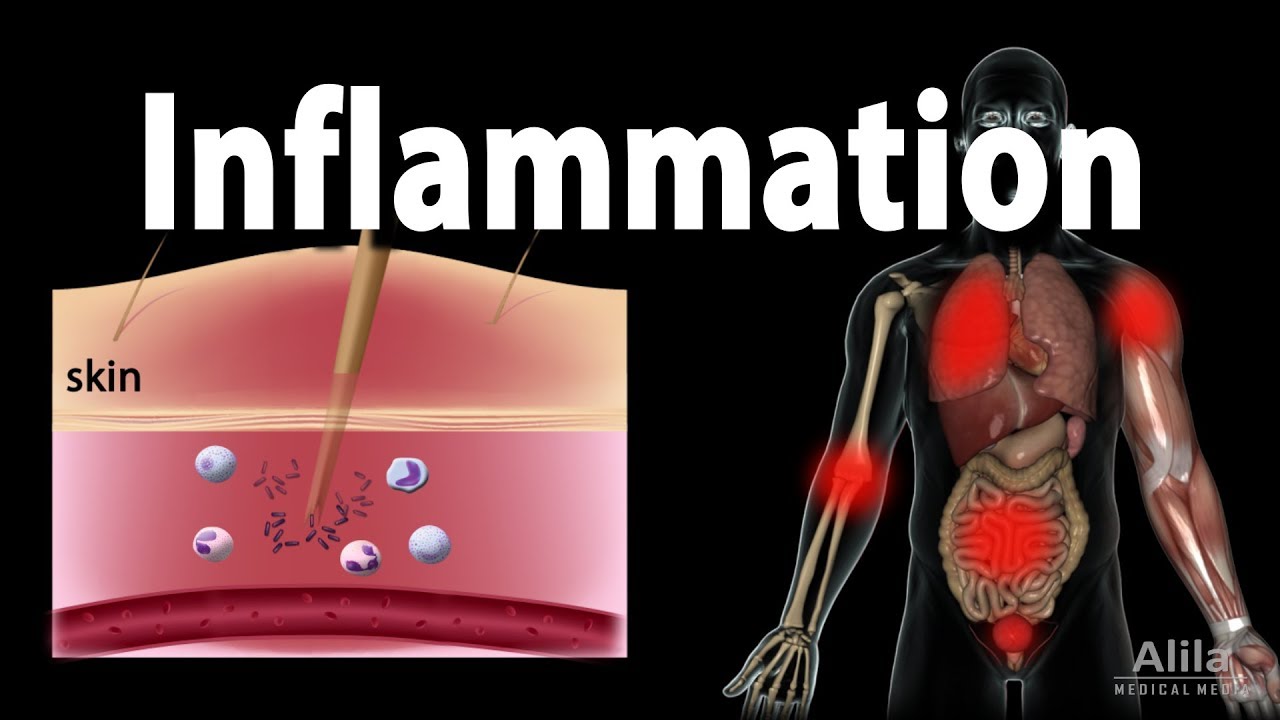
Inflammation - causes, symptoms, diagnosis, treatment, pathology
Summary
TLDRInflammation is the body's complex response to harmful stimuli like pathogens, toxins, or trauma, aiming to restore balance. It involves heat, pain, redness, and swelling, leading to temporary loss of function. Key players include macrophages, mast cells, and leukocytes, which release cytokines and other mediators to attract immune cells and initiate tissue repair. The innate immune response, activated by pattern recognition receptors, is rapid but non-specific. If mild, tissue regenerates; severe damage results in fibrous scarring.
Takeaways
- 🔍 Inflammation is characterized by four key signs: calor (heat), dolor (pain), rubor (redness), and tumor (swelling), which can lead to a fifth sign, functional lysa (temporary loss of function).
- 🌡 Inflammation is triggered by stimuli such as pathogens, toxins, or trauma, and is a response to restore balance and repair tissue damage.
- 🦠 Both external (like allergens and irritants) and internal (like DAMPs) factors can initiate inflammation, with microbial factors including virulence factors and PAMPs.
- 🛡 The immune system recognizes foreign substances through Pattern Recognition Receptors (PRRs), which activate leukocytes and initiate the inflammatory response.
- ⏰ The innate immune response is non-specific, rapid (occurring within minutes to hours), and lacks memory, distinguishing it from adaptive immunity.
- 🔬 There are two main types of leukocytes: granulocytes (like neutrophils and eosinophils) and agranulocytes (like lymphocytes and monocytes), which play crucial roles in inflammation.
- 🚨 Mast cells and macrophages are early responders in inflammation, releasing inflammatory mediators and increasing vascular permeability to allow immune cells to reach the site of injury.
- 🔄 Neutrophils are the first leukocytes to be recruited and they phagocytose pathogens, often leading to their own destruction in a process called neutrophil extracellular traps (NETs).
- 🩸 The complement system, activated by antibodies or pathogen molecules, aids in attracting leukocytes and optimizing pathogen phagocytosis, and can directly kill pathogens.
- 🛠️ Tissue repair involves macrophages clearing dead cells, angiogenesis for new blood vessel formation, and fibroblasts synthesizing collagen, leading to either tissue regeneration or scarring.
- 🔚 Inflammation concludes with tissue repair and resolution, aiming to restore tissue integrity or, in cases of severe damage, leaving a fibrous scar.
Q & A
What are the four classical signs of inflammation?
-The four classical signs of inflammation are calor (heat), dolor (pain), rubor (redness), and tumor (swelling).
What is the fifth sign sometimes associated with inflammation?
-The fifth sign sometimes associated with inflammation is functional lysa, which refers to a temporary loss of function due to pain or swelling.
What are the common causes of inflammation?
-Inflammation can be caused by pathogens, toxins, and trauma. For example, intense workouts can lead to muscle soreness due to inflammation.
What are the two main types of external factors that can trigger inflammation?
-The two main types of external factors that can trigger inflammation are non-microbial factors, such as allergens, irritants, and toxic compounds, and microbial factors.
What are the microbial factors that trigger inflammation?
-The microbial factors that trigger inflammation include virulence factors and pathogen-associated molecular patterns (PAMPs), which are small molecules shared across different pathogens.
What are Damage-Associated Molecular Patterns (DAMPs) and how do they relate to inflammation?
-DAMPs are intracellular proteins released when a cell's plasma membrane is injured or when a cell dies, signaling serious cell damage and triggering inflammation.
How do Pattern Recognition Receptors (PRRs) contribute to the inflammatory response?
-PRRs are cell surface receptors on leukocytes that recognize PAMPs and DAMPs, activating cells and sparking the inflammatory response.
What are the two main types of leukocytes involved in inflammation?
-The two main types of leukocytes involved in inflammation are granulocytes, which include neutrophils, eosinophils, basophils, and mast cells, and agranulocytes, which include lymphocytes and monocytes.
How do neutrophils contribute to the acute inflammatory process?
-Neutrophils are the first leukocytes recruited during the acute inflammatory process. They phagocytose pathogens and damaged cells, and then commit suicide to destroy the pathogens they've taken in.
What is the role of the complement system in inflammation?
-The complement system is a family of soluble proteins that get activated in the presence of antibodies or pathogen molecules. They help attract leukocytes, optimize phagocytosis, and directly kill pathogens by forming channels in their membranes.
How does the inflammatory response typically end?
-The inflammatory response typically ends with tissue repair, involving macrophages clearing dead cells, angiogenesis for new blood vessel formation, and fibroblasts synthesizing collagen for wound healing.
Outlines

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنMindmap

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنKeywords

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنHighlights

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنTranscripts

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنتصفح المزيد من مقاطع الفيديو ذات الصلة
5.0 / 5 (0 votes)