Nutrition in ICU
Summary
TLDRIn this presentation, Michal Pasz-durnick discusses the critical role of nutrition in ICU, emphasizing the balance between underfeeding and overfeeding. He reviews guidelines for starting nutrition, the preferred route, and calculating energy and protein needs. The talk highlights the importance of micronutrients, lipids, and carbohydrates in critical care nutrition and addresses specific nutrition approaches for various patient conditions.
Takeaways
- 🏥 **Critical Illness and Nutrition**: Critical illness leads to a hyper-metabolic state, increasing the risk of malnutrition. Proper nutrition support is vital for positive clinical outcomes.
- 📈 **Energy Requirements**: Accurate determination of a patient's energy requirements is crucial to prevent complications from underfeeding or overfeeding.
- 🕒 **Timing of Feeding**: Early enteral nutrition is recommended, with S-PEN suggesting within 48 hours and ASPEN between 24 to 48 hours.
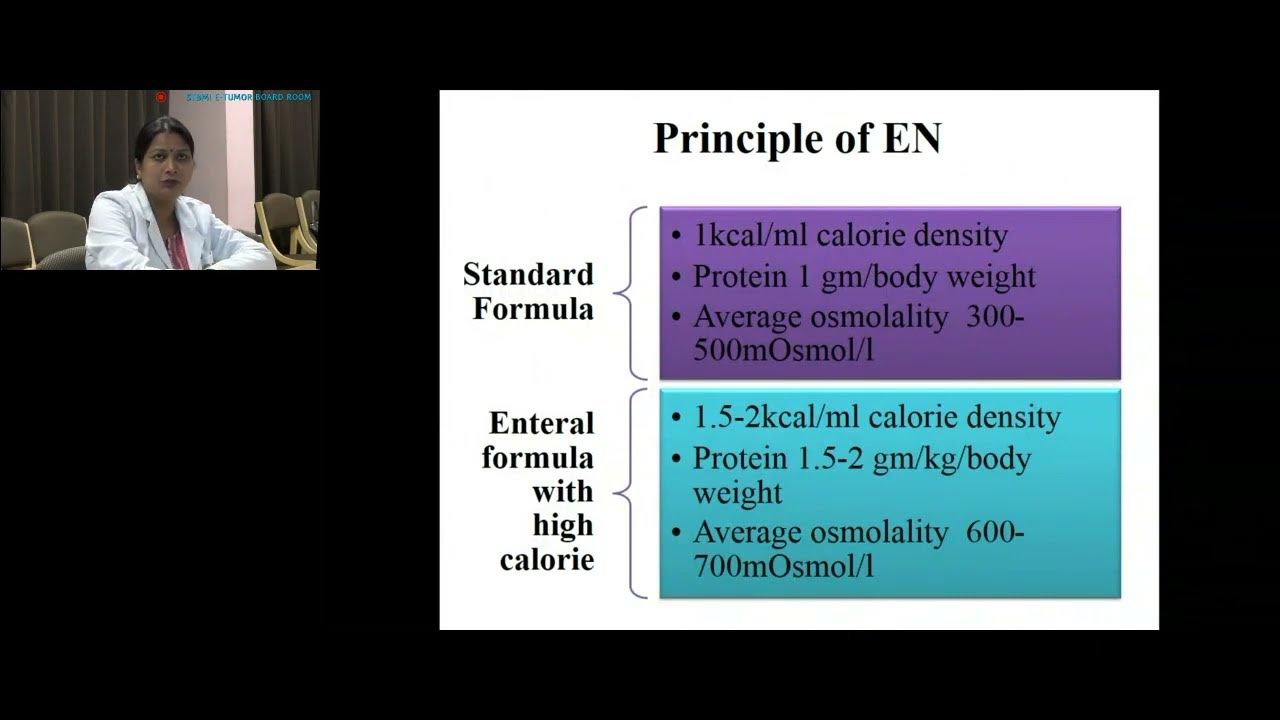
- 🥣 **Choice of Feeding Route**: Enteral nutrition is preferred, with parenteral nutrition used in high-risk aspiration cases.
- 🔍 **Energy Supply Calculation**: If indirect calorimetry isn't available, other methods like VO2 from pulmonary artery catheter or VCO2 from ventilator should be used.
- 💪 **Protein Intake**: Higher doses of protein are generally administered, with S-PEN recommending 1.3 to 1.5 grams/kg/day and ASPEN up to 2 grams/kg/day.
- 🚫 **No Strict Carbohydrate Dose**: There's no strict dose for carbohydrates, but ASPEN suggests a max dose of 5 mg/kg/min for critically ill patients.
- 🥃 **Lipid Dose**: The average lipid dose should be from 0.7 to 1.5 grams/kg/day, considering other sources of lipids.
- 🔬 **Indirect Calorimetry**: It's the gold standard for assessing energy expenditure but is not widely available, so alternative methods are discussed.
- 📊 **Predictive Equations**: These equations can be inaccurate, leading to over or underfeeding, hence indirect calorimetry is preferred.
- 📉 **Hypocaloric Nutrition**: In the early phase of acute illness, hypocaloric nutrition (not exceeding 70% of estimated or measured energy expenditure) should be administered.
- 📈 **Nutrient Quantification**: Nutrition dose should be based on the phase of critical illness, with adjustments made after day 3.
- 💊 **Micronutrients**: Essential for metabolism, immunity, and cell signaling, micronutrients should be provided daily with enteral nutrition.
Q & A
What is the significance of accurate determination of energy requirements in ICU patients?
-Accurate determination of energy requirements is crucial as nutrition support, including optimal energy supply, is key for positive clinical outcomes. Both underfeeding and overfeeding can lead to increased complications, hospital stays, and mortality rates.
According to the S-PEN guidelines, within how many hours should feeding in ICU patients begin?
-S-PEN recommends starting feeding within 48 hours.
What is the recommended timeframe for starting feeding according to ASPEN guidelines?
-ASPEN guidelines suggest starting feeding between 24 and 48 hours.
Why is enteral nutrition preferred over parenteral nutrition in high-risk aspiration patients?
-Enteral nutrition is preferred as it preserves intestinal epithelium, stimulates secretion of brush border enzymes, enhances immune function, and prevents bacterial translocation. Parenteral nutrition should be used in high-risk aspiration and gastric parasites.
How should energy supply be calculated if indirect calorimetry is not available?
-If indirect calorimetry is not available, energy expenditure should be estimated using VO2 from pulmonary artery catheter or VCO2 derived from the ventilator, as predictive equations can lead to significant inaccuracy.
What is the recommended protein intake per day for ICU patients as per S-PEN guidelines?
-S-PEN recommends a protein intake of 1.3 to 1.5 grams per kilogram per day.
What is the maximum dose of carbohydrates recommended by ASPEN guidelines for critically ill patients?
-ASPEN guidelines recommend a maximum dose of 5 milligrams per kilogram per minute of carbohydrates, with lower doses being desirable for certain patients.
Why is it important to monitor glycemia levels in ICU patients receiving nutrition?
-Glycemia should always be below 10 millimoles per liter to prevent complications associated with hyperglycemia.
What are the potential complications of overfeeding in ICU patients?
-Overfeeding can lead to hyperglycemia, hypertriglyceridemia, hepatic steatosis, azotemia, hypercapnia, and increased mortality rates.
When should supplemental parenteral nutrition be considered according to ASPEN guidelines?
-Supplemental parenteral nutrition should be considered in patients who do not tolerate full dose of enteral nutrition during the first week in the ICU, with safety and benefits weighed on a case-by-case basis.
What is the recommended approach for nutrition in intubated patients with gastrointestinal motility issues?
-Gastric access should be used as the standard approach to initiate enteral nutrition. For patients with high risk of aspiration or intolerance of gastric administration, anterior nutrition is recommended with gentle administration.
Outlines

此内容仅限付费用户访问。 请升级后访问。
立即升级Mindmap

此内容仅限付费用户访问。 请升级后访问。
立即升级Keywords

此内容仅限付费用户访问。 请升级后访问。
立即升级Highlights

此内容仅限付费用户访问。 请升级后访问。
立即升级Transcripts

此内容仅限付费用户访问。 请升级后访问。
立即升级浏览更多相关视频
Nutrition in ICU by Shilpi Pandey, SGPGIMS, Lucknow

MATA KULIAH ILMU GIZI PERKENALAN

Zach Bitter's Low-Carb Nutrition Approach for Running

DESAIN GRAFIS CANVA - MENGENAL LAYOUT

Menelusuri konsep dan urgensi harmoni kewajiban dan hak negara dan warga negara @johnykoynja

Roles & Differences between Architecture Urban Planning & Urban Design Ar Priyanka Dumane
5.0 / 5 (0 votes)
