Alzheimer’s Disease — Managing Stages of Dementia | NEJM
Summary
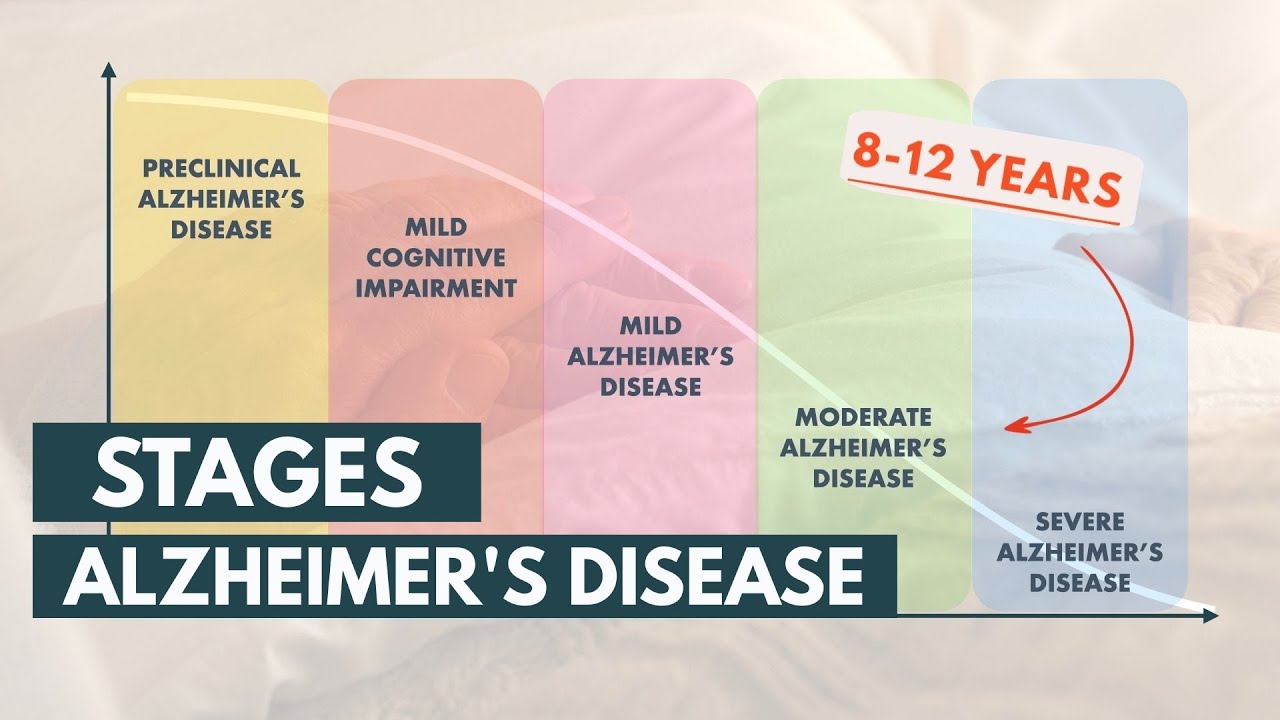
TLDRThis script delves into the nuances of cognitive diseases like mild cognitive impairment and dementia, highlighting the importance of functional differences in diagnosis and treatment. It emphasizes the role of early diagnosis, the impact on daily activities, and the necessity of support systems for patients and caregivers. The discussion also covers the progression of the disease, the use of medications, and the importance of advanced care planning, while acknowledging the challenges and stressors faced by caregivers.
Takeaways
- 🧠 Function is the key differentiator between mild cognitive impairment and dementia, with the latter involving a functional impairment.
- 👨🏫 The speaker transitioned from a CEO to having a first-grade level math equivalency due to cognitive decline, highlighting the impact of cognitive diseases on daily life.
- 🏠 Geriatricians focus on both basic and instrumental activities of daily living, with the latter being more complex and often affected earlier in the progression of cognitive diseases.
- 🛑 Early diagnosis of cognitive impairment is crucial for initiating treatments and support to maintain independence and quality of life.
- 📝 Keeping a routine, staying socially engaged, and maintaining physical and mental health are essential for managing early-stage cognitive diseases.
- 👨👩👧👦 Support from family and friends, as well as community organizations, is vital for individuals with cognitive impairments and their caregivers.
- 📝 The importance of having advanced directives and discussing end-of-life care preferences early on in the disease process.
- 🚫 Safety concerns are paramount, especially as cognitive function declines, affecting areas such as medication management, finances, and driving.
- 🔑 The transition to moderate dementia often requires more support and may involve difficult decisions like activating health care proxies and considering assisted living.
- 💊 Medications for dementia aim to slow cognitive decline, but their benefits and side effects must be carefully weighed against the stage of the disease.
- 🛑 The progressive nature of dementia means increasing demands on caregivers, emphasizing the importance of self-care and access to support resources.
Q & A
What is the primary distinction between mild cognitive impairment and dementia according to the script?
-The primary distinction is based on functionality. Mild cognitive impairment involves symptoms but maintains functional independence, whereas dementia is characterized by functional impairment where individuals can no longer perform tasks they previously could.
How does the speaker's personal experience with cognitive decline manifest in their professional life?
-The speaker went from being a CEO in finance and real estate to having a first-grade level math equivalency, indicating significant cognitive decline that affected their ability to perform professional tasks.
What are the basic activities of daily living mentioned in the script?
-The basic activities of daily living include turning in bed, standing up, walking, going to the bathroom, using the bathroom, bathing, brushing teeth, dressing, and eating.
What are instrumental activities of daily living, and why are they significant in the context of cognitive diseases?
-Instrumental activities of daily living are more complex tasks such as making appointments, managing medications, finances, driving, cooking, cleaning, and using technology. They are significant because changes in the ability to perform these tasks often indicate a transition from mild cognitive impairment to dementia.
Why is it important to focus on functional changes in early-stage cognitive diseases?
-Focusing on functional changes is important for early detection of dementia, allowing for earlier intervention with medications, support groups, and community involvement, which can help manage the disease more effectively.
What is the significance of early diagnosis in managing cognitive diseases?
-Early diagnosis allows individuals to make clear their wishes regarding their care, such as preferences for staying at home or moving to a care facility, and to establish advanced directives like living wills and power of attorney.
How can family members support someone with mild cognitive impairment in their daily life?
-Family members can support by ensuring the individual is on a routine, socially engaged, maintaining good physical and mental health, and staying connected to care. Simple reminders, like text messages, can also be helpful.
What are some practical steps the speaker took to cope with their cognitive impairment?
-The speaker used strategies like setting alarms, utilizing technology like Alexa, arranging for Uber rides, and keeping a pad by the bed to make lists of tasks for the next day to prevent forgetting.
What is the role of medication in managing dementia, and how is it discussed with patients?
-Medication can help slow the progression of dementia and maintain day-to-day function. It's important to discuss realistic expectations, potential side effects, and the benefits of medication at different stages of the disease with patients.
What are the considerations for caregivers when deciding whether home care is still appropriate for a loved one with dementia?
-Caregivers must consider the physical and mental health of the individual, the ability to swallow and manage incontinence, language decline, and overall safety at home. They may need to discuss the possibility of skilled nursing or hospice care with a physician.
How does the speaker address the challenges and stress of caregiving for someone with dementia?
-The speaker acknowledges the difficulty and fluctuation of caregiving, emphasizing the importance of self-care, honest communication with healthcare providers, and seeking support from resources like the Alzheimer's Association and community services.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Early Detection and Management of Mild Cognitive Impairment
Stages and Life Expectancy of Alzheimer's Disease

AI for Mental Health FCAI 23 5 2024 Hanna Renvall HUS BioMag Laboratory

STOP Doing THIS! Your Dementia Risk Skyrockets By 80%

Podcast: A Healthy Brain Is a Happy Brain

Delier en Dementie: overeenkomsten en verschillen
5.0 / 5 (0 votes)