Hemodialysis
Summary
TLDRThis video provides an in-depth overview of the complications that can occur during and after hemodialysis. Key issues include vascular access problems, infections, bleeding, hypotension, muscle cramps, nausea, and vomiting. The transcript also highlights the importance of proper care and monitoring, especially to prevent serious conditions like Disequilibrium Syndrome, which can cause neurological complications. Adjustments in dialysis settings and timely intervention are crucial for ensuring patient safety and effective treatment.
Takeaways
- 😀 Proper vascular access care is critical in hemodialysis, as any compromise can lead to serious complications like clots, stenosis, or infection.
- 😀 Patients should avoid tight clothing, wearing jewelry, or sleeping on the side of the fistula to protect the vascular access point from damage.
- 😀 Infection at the vascular access site can render it unusable, requiring alternative dialysis methods like a central venous catheter.
- 😀 Underlying infections (e.g., UTI, respiratory infections) may not be immediately apparent but can complicate dialysis and worsen patient outcomes.
- 😀 Hemorrhaging and bleeding are possible complications due to the use of anticoagulants during dialysis, requiring careful monitoring of the access point.
- 😀 Hypotension may occur during dialysis if the treatment rate is too high or if fluid levels are not managed properly, requiring adjustments.
- 😀 Muscle cramps can develop from rapid fluid and electrolyte changes during dialysis, and addressing imbalances can help alleviate these symptoms.
- 😀 Nausea and vomiting during dialysis may indicate a problem, including disequilibrium syndrome or other underlying health issues.
- 😀 Disequilibrium syndrome can occur when fluids and electrolytes are adjusted too rapidly, leading to serious complications like cerebral edema or increased intracranial pressure.
- 😀 Quick identification and intervention are essential in managing disequilibrium syndrome to prevent severe outcomes like confusion, seizures, or loss of consciousness.
- 😀 Dialysis treatment requires close monitoring of patient symptoms and lab results to ensure the appropriate adjustments are made for safety and efficacy.
Q & A
What is the most important concern for patients undergoing hemodialysis?
-The most important concern is maintaining the vascular access point. This access is essential for dialysis, and any complications like clotting, stenosis, or infection can lead to the loss of access, which would require additional procedures and potentially a central venous catheter.
Why are patients on anticoagulants during hemodialysis?
-Patients are on anticoagulants to prevent the formation of clots at the vascular access site. This helps ensure that the dialysis process runs smoothly, as clots could block the access and cause complications.
What actions can compromise the health of the vascular access site?
-Actions like wearing tight clothing or jewelry, having blood pressure taken on the access side, or carrying heavy objects can all compromise the health of the vascular access site. These activities can cause pressure or trauma that impairs circulation or healing.
What complications can arise if an infection occurs at the vascular access site?
-An infection at the vascular access site can render the access unusable for dialysis. This could prevent dialysis from being performed and lead to the need for additional procedures or even the placement of a central venous catheter.
What are the signs that a patient might have an underlying infection during dialysis?
-Signs of an underlying infection include a spike in temperature, rapid decline in condition, increased breathing rate, and visible symptoms like redness, swelling, or pus around the access point. These symptoms suggest the patient may have an infection, such as a UTI or respiratory infection.
How does rapid dialysis affect a patient's blood pressure?
-Rapid dialysis can lower a patient's blood pressure, especially if fluid is removed too quickly. This can lead to hypotension, dizziness, fainting, and other complications. Adjusting the rate of dialysis can help prevent or manage this issue.
What is the role of fluid and electrolyte management in preventing muscle cramps during dialysis?
-Muscle cramps during dialysis are often caused by rapid changes in fluid and electrolyte levels. Monitoring and adjusting these levels, along with providing medications or gentle stretching, can help reduce the occurrence of muscle cramps.
What might nausea and vomiting indicate in a dialysis patient?
-Nausea and vomiting in a dialysis patient could be a result of rapid fluid shifts, but it might also signal an underlying issue like disequilibrium syndrome, which requires immediate attention. If symptoms don't improve with antiemetic treatment, further investigation is needed.
What is disequilibrium syndrome, and why is it a concern during dialysis?
-Disequilibrium syndrome occurs when fluid and electrolyte changes during dialysis are too rapid, leading to cerebral edema (brain swelling) and increased intracranial pressure. This can cause nausea, vomiting, confusion, and even seizures, making it a medical emergency that needs prompt intervention.
What are the potential consequences of untreated disequilibrium syndrome?
-If left untreated, disequilibrium syndrome can progress to more severe symptoms, including altered mental status, confusion, and even loss of consciousness or seizures. Early identification and treatment are critical to prevent these dangerous outcomes.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video

Manajemen Cairan Pada Pasien Gagal Ginjal yang Menjalani Cuci Darah oleh dr. Ruwaeda Nasruddin

TUTORIAL CARA MENGOPERASIKAN MESIN CUCI DARAH (HEMODIALISA) || DUNIA KEPERAWATAN
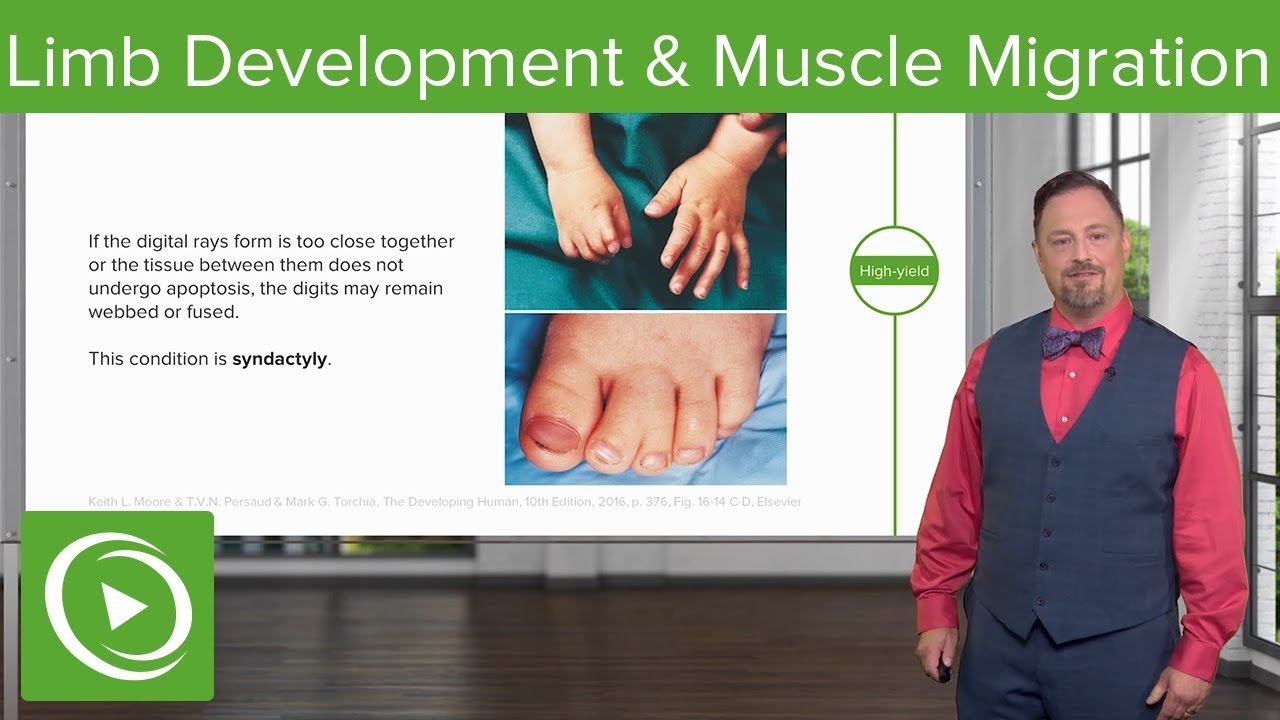
Limb Development and Muscle Migration – Embryology | Lecturio

Down Syndrome, Causes, Signs and Symptoms, Diagnosis and Treatment.

Pregnancy - physiology

Identifying common hemodialysis access complications
5.0 / 5 (0 votes)