Understanding Open Angle Glaucoma
Summary
TLDRThis video by Zero to Finals covers open-angle glaucoma, a condition caused by increased intraocular pressure leading to optic nerve damage. The presenter explains the anatomy and physiology of the eye, focusing on the flow of aqueous humor and its role in maintaining eye pressure. The video discusses the causes, symptoms, and diagnosis of open-angle glaucoma, highlighting risk factors like age, family history, and myopia. Treatments include eye drops, beta blockers, and surgical procedures, aiming to reduce pressure and prevent further vision loss.
Takeaways
- 📈 Glaucoma refers to optic nerve damage caused by increased intraocular pressure.
- 👁️ Open-angle glaucoma involves a gradual increase in resistance through the trabecular meshwork, causing a slow rise in eye pressure.
- 💡 The aqueous humor flows from the ciliary body through the anterior chamber and drains via the trabecular meshwork into the canal of Schlemm.
- 🔍 Normal intraocular pressure ranges from 10 to 21 mmHg, and higher pressures indicate increased resistance to aqueous humor flow.
- 👓 Risk factors for open-angle glaucoma include age, family history, black ethnic origin, and nearsightedness (myopia).
- 👁️🗨️ Open-angle glaucoma often presents without symptoms but can lead to gradual peripheral vision loss, tunnel vision, and night-time halos around lights.
- 🩺 Two common methods to measure intraocular pressure include non-contact tonometry (air puff test) and Goldman applanation tonometry (more accurate).
- 🔬 Diagnosis of glaucoma involves checking intraocular pressure, optic disc cupping, and visual field assessment for peripheral vision loss.
- 💧 First-line treatment involves prostaglandin analogs like latanoprost, which increase the outflow of aqueous humor and reduce pressure.
- 🔧 Surgery, such as trabeculectomy, may be needed when eye drops are ineffective, creating a new drainage channel for aqueous humor.
Q & A
What is glaucoma, and how is it related to intraocular pressure?
-Glaucoma refers to optic nerve damage caused by a significant rise in intraocular pressure (IOP). Elevated IOP occurs due to a blockage in the drainage of aqueous humor from the eye, leading to increased pressure.
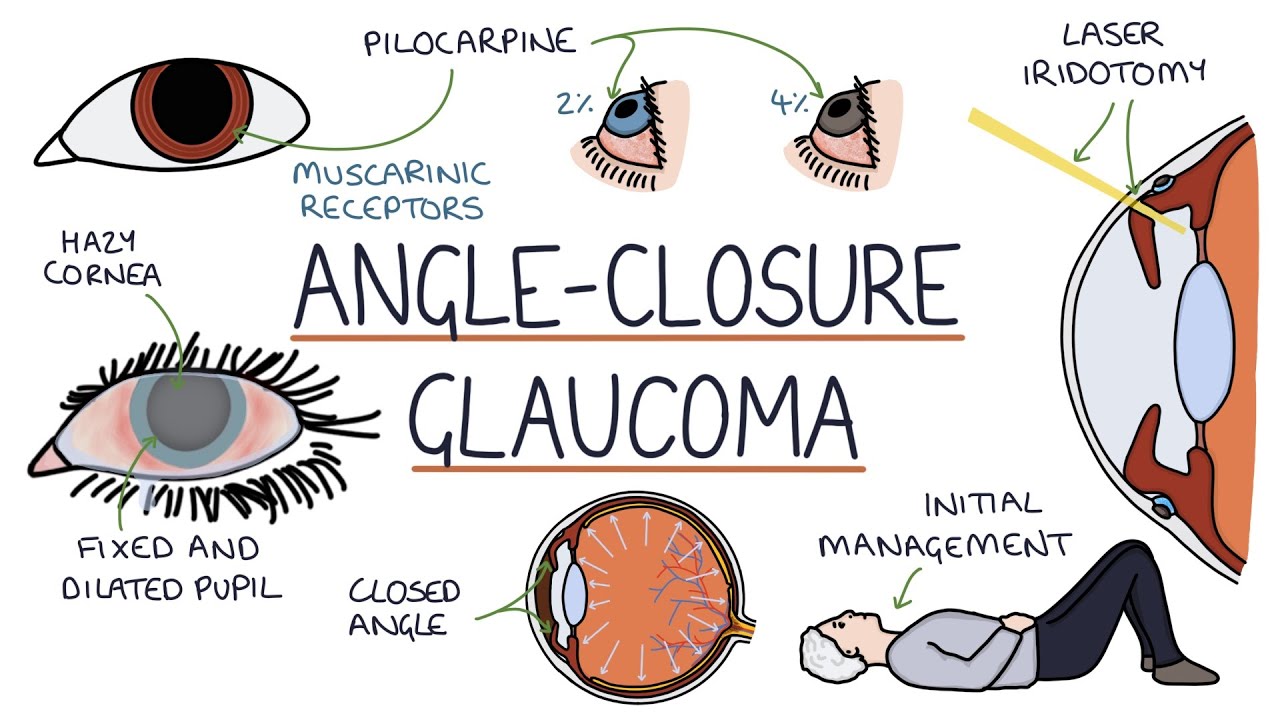
What are the two main types of glaucoma, and which type is discussed in the video?
-The two main types of glaucoma are open-angle and closed-angle glaucoma. The video focuses on open-angle glaucoma, where the resistance to the outflow of aqueous humor through the trabecular meshwork increases gradually.
How does aqueous humor flow through the eye, and how is it related to intraocular pressure?
-Aqueous humor is produced by the ciliary body, flows from the posterior chamber to the anterior chamber, and drains through the trabecular meshwork into the canal of Schlemm. Resistance to this outflow creates intraocular pressure; if the resistance increases, the IOP rises.
What is the normal range of intraocular pressure, and what happens when this pressure increases in open-angle glaucoma?
-The normal intraocular pressure is between 10 to 21 mmHg. In open-angle glaucoma, increased resistance in the trabecular meshwork leads to a gradual rise in pressure, causing damage to the optic nerve over time.
What is optic disc cupping, and how is it associated with glaucoma?
-Optic disc cupping occurs when raised intraocular pressure causes the optic cup (a small indent in the optic disc) to become larger and deeper. An optic cup greater than 0.5 the size of the optic disc is considered abnormal and may indicate glaucoma.
What are the key risk factors for developing open-angle glaucoma?
-Risk factors for open-angle glaucoma include increasing age, family history of glaucoma, black ethnic origin, and myopia (nearsightedness).
How does open-angle glaucoma typically present, and what are the common symptoms?
-Open-angle glaucoma often presents asymptomatically, with a gradual loss of peripheral vision (tunnel vision), fluctuating pain, headaches, blurred vision, and halos around lights, especially at night.
What are the methods used to measure intraocular pressure, and how do they work?
-Intraocular pressure is measured using non-contact tonometry, which estimates IOP by shooting a puff of air at the cornea, and Goldmann applanation tonometry, the gold standard, which applies pressure to the cornea to get an accurate measurement.
How is open-angle glaucoma diagnosed?
-Diagnosis involves measuring intraocular pressure with Goldmann applanation tonometry, assessing optic disc cupping through fundoscopy, and checking for peripheral vision loss using visual field tests.
What are the treatment options for managing open-angle glaucoma?
-Treatment aims to reduce intraocular pressure. First-line treatment includes prostaglandin analogs like latanoprost, which increase uveoscleral outflow. Other options include beta blockers, carbonic anhydrase inhibitors, sympathomimetics, and surgical procedures like trabeculectomy if eye drops are ineffective.
Outlines

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowMindmap

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowKeywords

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowHighlights

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowTranscripts

This section is available to paid users only. Please upgrade to access this part.
Upgrade NowBrowse More Related Video
5.0 / 5 (0 votes)