Pharmacology - HYPERTENSION & ANTIHYPERTENSIVES (MADE EASY)
Summary
TLDRThis lecture delves into the pharmacology of antihypertensive drugs, explaining the physiological basis of blood pressure regulation and the role of systems like baroreceptors and the renin-angiotensin-aldosterone system. It outlines various drug classes that target these mechanisms, such as alpha-1 blockers, beta blockers, calcium channel blockers, diuretics, and drugs affecting the renin-angiotensin-aldosterone system, to reduce blood pressure. The lecture also touches on side effects and other agents like Bosentan and Fenoldopam, providing a comprehensive overview of hypertension management.
Takeaways
- 💡 Hypertension is a common disorder often without noticeable symptoms and is related to the force of blood against artery walls.
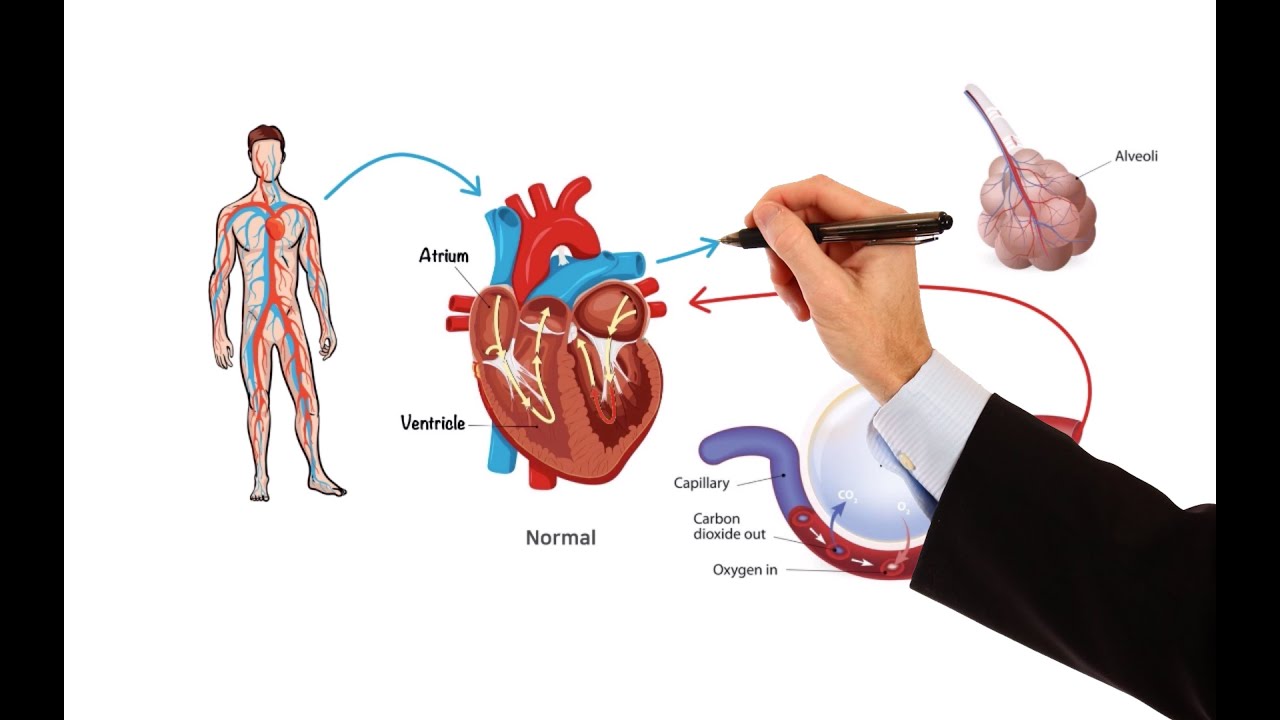
- 🌡 Blood pressure is maintained by factors such as cardiac output, systemic vascular resistance, arterial wall elasticity, and blood volume.
- 🔍 Baroreceptors in the aortic arch and carotid sinuses are key in blood pressure regulation, responding to changes and triggering the release of catecholamines.
- 🏋️♂️ Beta-1 receptor activation increases heart rate and stroke volume, boosting cardiac output and blood pressure.
- 🌀 Alpha-1 receptor activation leads to vasoconstriction, increasing vascular resistance and blood pressure.
- 🚰 The renin-angiotensin-aldosterone system plays a significant role in blood pressure regulation, with renin initiating the production of angiotensin II, a potent vasoconstrictor.
- 🛡️ Antihypertensive drugs work by disrupting different aspects of the blood pressure regulation system, with classes including alpha-1 blockers, beta blockers, and others.
- 💊 Alpha-1 blockers like Doxazosin reduce systemic vascular resistance and blood pressure by blocking alpha-1 receptors on smooth muscle.
- 💓 Selective beta blockers such as Atenolol decrease cardiac output by blocking beta-1 receptors on the heart, thus lowering blood pressure.
- 🧠 Centrally acting adrenergic drugs like Clonidine work by reducing sympathetic activity in the brain, leading to decreased blood pressure.
- 💊 Calcium channel blockers, divided into dihydropyridines and nondihydropyridines, reduce blood pressure by inhibiting calcium entry into smooth muscle cells or cardiac cells, respectively.
- 🌿 Diuretics are categorized into loop, thiazide, and potassium-sparing, each reducing blood pressure through different mechanisms involving sodium and water balance in the body.
- 🛑 Drugs targeting the renin-angiotensin-aldosterone system, such as renin inhibitors, ACE inhibitors, and ARBs, lower blood pressure by reducing angiotensin II production or its effects.
- 🚑 Other antihypertensive agents not fitting into the main classes include Bosentan for pulmonary hypertension, Fenoldopam for short-term severe hypertension management, and direct-acting smooth muscle relaxants like Hydralazine.
Q & A
What is hypertension and why is it often asymptomatic?
-Hypertension, also known as high blood pressure, is a common disorder that affects many people. It is often asymptomatic, meaning that individuals typically do not notice any symptoms, which can make it challenging to detect without regular monitoring.
How is blood pressure maintained in the body?
-Blood pressure is maintained by several factors including the contraction of the left ventricle, systemic vascular resistance, elasticity of the arterial walls, and blood volume. It is essentially the product of cardiac output and systemic vascular resistance.
What are baroreceptors and how do they regulate blood pressure?
-Baroreceptors are pressure-sensitive neurons located in the aortic arch and carotid sinuses. They regulate blood pressure by sending signals to the adrenal medulla when blood pressure falls too low, causing the release of catecholamines and increasing sympathetic activity.
How does the renin-angiotensin-aldosterone system contribute to blood pressure regulation?
-The renin-angiotensin-aldosterone system plays a significant role in blood pressure regulation. When blood pressure or blood flow to the kidneys falls, baroreceptors in the kidneys release renin, which is necessary for the production of angiotensin II, a potent vasoconstrictor that increases peripheral resistance and blood volume, ultimately leading to increased blood pressure.
What are alpha-1 blockers and how do they affect blood pressure?
-Alpha-1 blockers, such as Doxazosin and Prazosin, work by blocking alpha-1 receptors on smooth muscle, leading to a decrease in systemic vascular resistance and, consequently, a decrease in blood pressure.
What is the role of beta blockers in treating hypertension?
-Beta blockers, such as Atenolol and Metoprolol, selectively block beta-1 receptors on the heart, reducing cardiac output and thereby decreasing blood pressure. Non-selective beta blockers like Labetalol and Carvedilol can also block alpha-1 receptors, further decreasing vascular resistance.
How do centrally acting adrenergic drugs lower blood pressure?
-Centrally acting adrenergic drugs, such as Clonidine and Methyldopa, work by blocking sympathetic activity within the brain. They stimulate presynaptic alpha-2 receptors, reducing catecholamine production and release, which leads to decreased systemic vascular resistance and cardiac output, and ultimately lowers blood pressure.
What are calcium channel blockers and how do they impact blood pressure?
-Calcium channel blockers are divided into dihydropyridines and nondihydropyridines. Dihydropyridines selectively inhibit L-type calcium channels in vascular smooth muscle, reducing vascular resistance and blood pressure. Nonditihydropyridines block calcium channels in both vascular smooth muscle and cardiac cells, leading to reduced myocardial contractility, slower heart rate, and vasodilation, which also contributes to lowering blood pressure.
What are the different types of diuretics and how do they treat hypertension?
-Diuretics used in hypertension treatment include loop diuretics, thiazide diuretics, and potassium-sparing diuretics. Loop diuretics like Furosemide reduce sodium chloride reabsorption, leading to significant diuresis and decreased blood pressure. Thiazide diuretics reduce sodium chloride reabsorption to a lesser extent and are thought to produce sustained antihypertensive effects through vasodilation. Potassium-sparing diuretics either interfere with sodium potassium exchange in the kidneys or block aldosterone actions, increasing diuresis and often used in combination with other diuretics to prevent potassium loss.
How do agents that work on the renin-angiotensin-aldosterone system reduce blood pressure?
-Agents that work on the renin-angiotensin-aldosterone system reduce blood pressure by either inhibiting the production of angiotensin II or blocking its actions on the AT1 receptors. This leads to decreased systemic vascular resistance without significant changes in cardiac output and also improves renal blood flow, reducing the risk of renal injury.
What are some side effects associated with the use of dihydropyridines?
-Side effects of dihydropyridines, which are related to systemic vasodilation, can include dizziness, headache, flushing, peripheral edema, and in some cases, gingival hyperplasia, or swelling of the gums.
What are the potential side effects of ACE inhibitors?
-ACE inhibitors may cause dry cough and, in rare cases, angioedema, which can be life-threatening. These side effects are thought to be due to increased levels of bradykinin and substance P resulting from the inhibition of the angiotensin-converting enzyme.
What is unique about the mechanism of action of Fenoldopam in treating hypertension?
-Fenoldopam is a selective dopamine-1 receptor agonist that produces generalized arterial vasodilation, leading to decreased peripheral resistance and lower blood pressure. It also inhibits tubular sodium reabsorption, resulting in natriuresis and diuresis. Due to its rapid onset and short duration of action, Fenoldopam is often used in hospitals for the short-term management of severe hypertension.
Outlines

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードMindmap

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードKeywords

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードHighlights

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレードTranscripts

このセクションは有料ユーザー限定です。 アクセスするには、アップグレードをお願いします。
今すぐアップグレード関連動画をさらに表示

Antihipertensi (2): Fisiologi pengaturan tekanan darah

Fisiologi Pengaturan Tekanan Darah

Renin-Angiotensin-Aldosterone System (RAA System) | Made easy with a step-by-step explanation!
Pharmacology – HEART FAILURE (MADE EASY)

Sistema renina angiotensina aldosterona

Renin Angiotensin Aldosterone System | RAAS | Juxtaglomerular Apparatus | JGA | Renal Physiology
5.0 / 5 (0 votes)
