Pharmacology – HEART FAILURE (MADE EASY)
Summary
TLDRThis lecture delves into the pharmacology of drugs used in treating heart failure. It covers the heart's function, the physiological mechanisms that fail in heart failure, and compensatory responses such as the activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system. The lecture then explores various drug classes used in treatment, including beta-blockers, ACE inhibitors, ARBs, angiotensin receptor-neprilysin inhibitors, aldosterone antagonists, diuretics, vasodilators, and digoxin. Each class is explained in terms of its mechanism of action and how it alleviates symptoms or reduces mortality in heart failure patients.
Takeaways
- 😀 Heart failure is a chronic and progressive condition where the heart cannot pump enough blood to meet the body's needs.
- 😀 The heart operates in four major steps: right atrium receives oxygen-poor blood, right ventricle pumps it to the lungs, left atrium receives oxygen-rich blood, and left ventricle pumps it to the body.
- 😀 The Frank-Starling law describes how increased blood volume leads to stronger heart contractions, but this mechanism fails in heart failure, reducing efficiency.
- 😀 Heart failure can be classified into systolic heart failure (HFrEF) with reduced ejection fraction and diastolic heart failure (HFpEF) with preserved ejection fraction.
- 😀 The body compensates for heart failure by increasing sympathetic nervous system activity and activating the renin-angiotensin-aldosterone system (RAAS).
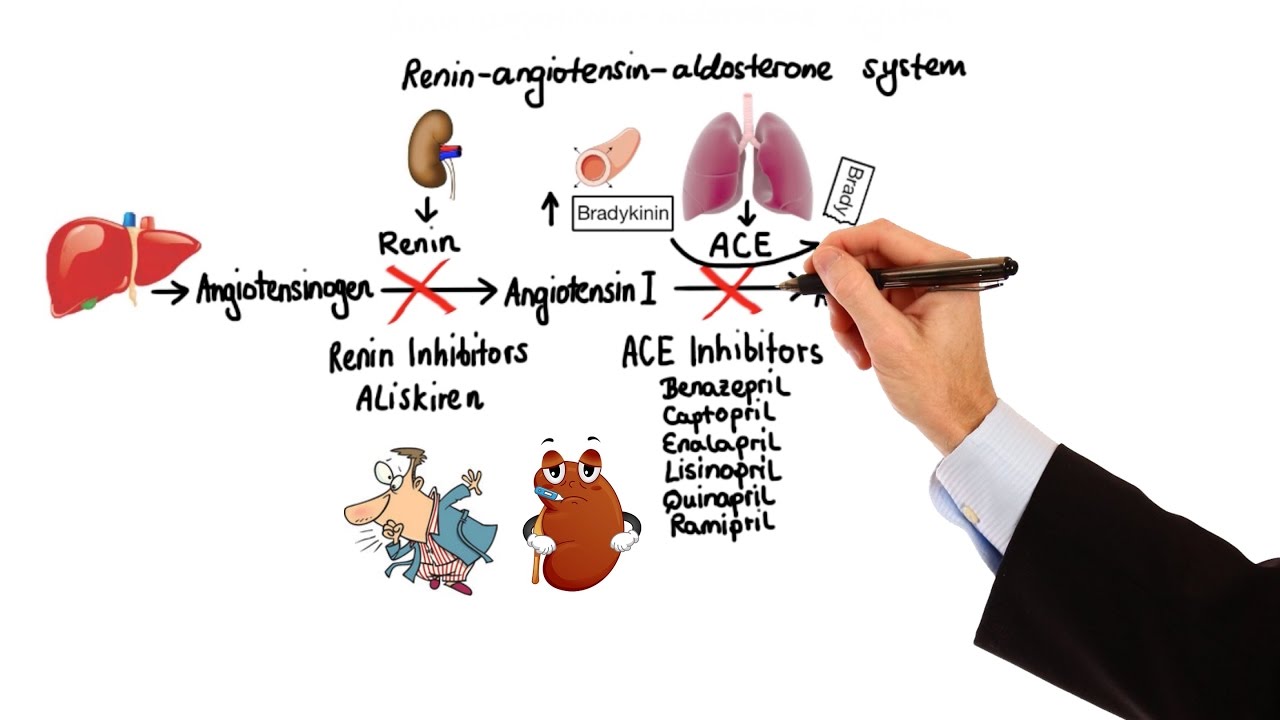
- 😀 The RAAS pathway includes the release of renin, conversion of angiotensin I to angiotensin II, leading to vasoconstriction, fluid retention, and increased blood pressure.
- 😀 Natriuretic peptides (ANP, BNP, CNP) are secreted to counteract volume overload, promote sodium and water excretion, and inhibit the effects of the RAAS and sympathetic nervous system.
- 😀 The pharmacological treatment of heart failure includes beta-blockers, ACE inhibitors, angiotensin receptor blockers (ARBs), neprilysin inhibitors, aldosterone antagonists, loop diuretics, and vasodilators.
- 😀 Beta-blockers (e.g., Bisoprolol, Carvedilol, Metoprolol) reduce heart rate and contractility, improving blood flow and reducing mortality in heart failure patients.
- 😀 ACE inhibitors (e.g., Enalapril, Lisinopril) lower angiotensin II levels, causing vasodilation and reducing blood pressure, which relieves heart strain.
- 😀 Digoxin increases cardiac output by enhancing heart muscle contractility through inhibition of the sodium-potassium ATPase pump, raising intracellular calcium levels.
Q & A
What is heart failure, and how does it impact the heart's ability to function?
-Heart failure is a chronic and progressive disorder where the heart muscle is unable to pump enough blood to meet the body's needs. The heart's function is compromised due to reduced ability to effectively contract or relax, which leads to insufficient blood flow to vital organs.
What is the Frank-Starling law, and how is it affected by heart failure?
-The Frank-Starling law states that the heart pumps out as much blood as it receives, with increased ventricular filling leading to a stronger contraction and greater cardiac output. In heart failure, this mechanism fails because the heart muscle becomes less efficient, and excessive blood in the ventricle reduces contraction effectiveness.
What is the difference between systolic and diastolic heart failure?
-In systolic heart failure, the heart muscle is weak and cannot squeeze enough blood out, leading to reduced ejection fraction (less than 40%). Diastolic heart failure occurs when the heart muscle is stiff and cannot relax properly to allow for adequate ventricular filling, though ejection fraction remains normal.
How does the body try to compensate for reduced cardiac output in heart failure?
-The body compensates by increasing sympathetic nervous system activity, which increases heart rate and contractility. It also activates the renin-angiotensin-aldosterone system (RAAS) to raise blood pressure and maintain blood volume, attempting to improve perfusion to vital organs.
What role does the sympathetic nervous system play in heart failure?
-In heart failure, the sympathetic nervous system is activated to increase heart rate and contractility through the release of norepinephrine. This response tries to boost cardiac output by increasing stroke volume and heart rate to maintain adequate blood pressure.
How does the renin-angiotensin-aldosterone system (RAAS) contribute to heart failure progression?
-RAAS is activated in heart failure to raise blood pressure and volume. Renin triggers the production of angiotensin II, which leads to vasoconstriction, increased aldosterone release, sodium and water retention, and ultimately contributes to increased blood pressure, edema, and additional strain on the heart.
What are natriuretic peptides, and how do they help in heart failure?
-Natriuretic peptides (ANP, BNP, CNP) are released in response to myocardial stretch and volume overload. They counteract the effects of RAAS and sympathetic activation by promoting sodium and water excretion, relaxing the myocardium, and inhibiting cardiac hypertrophy, fibrosis, and vasoconstriction.
How do beta-blockers help in managing heart failure?
-Beta-blockers help by blocking beta-1 receptors, reducing heart rate and contractility, which decreases cardiac output and blood pressure. This reduces the workload on the heart and improves diastolic filling time. Certain beta-blockers also reduce renin secretion, indirectly lowering blood pressure.
What are ACE inhibitors, and how do they assist in heart failure treatment?
-ACE inhibitors block the angiotensin-converting enzyme, reducing the production of angiotensin II. This lowers vasoconstriction, blood pressure, and fluid retention. Additionally, ACE inhibitors increase bradykinin levels, which promotes vasodilation, further aiding in lowering blood pressure and relieving strain on the heart.
What is the role of aldosterone antagonists in heart failure treatment?
-Aldosterone antagonists, like Spironolactone and Eplerenone, block aldosterone's effects by preventing its binding to mineralocorticoid receptors. This reduces sodium and water retention and potassium excretion, leading to beneficial effects on fluid balance, blood pressure, and heart protection in heart failure patients.
Outlines

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنMindmap

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنKeywords

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنHighlights

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنTranscripts

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنتصفح المزيد من مقاطع الفيديو ذات الصلة

Pharmacology - ADRENERGIC RECEPTORS & AGONISTS (MADE EASY)

Pharmacology - ANTIPSYCHOTICS (MADE EASY)

Curso de Farmacologia: Aula 7 - Farmacologia adrenergica - Agonistas e antagonistas diretos

Vasopressor Drugs (Medical Definition) | Quick Explainer Video

Pharmacology - GASTROINTESTINAL AND ANTIEMETIC DRUGS (MADE EASY)
Pharmacology - HYPERTENSION & ANTIHYPERTENSIVES (MADE EASY)
5.0 / 5 (0 votes)
