Transverse Myelitis
Summary
TLDRThis video explains transverse myelitis, an inflammatory condition affecting the spinal cord that leads to demyelination and potential neuron damage. It covers the disease's causes (peri-infectious, autoimmune, and idiopathic), the involvement of T cells in inflammation, and its clinical features like sensory loss, motor dysfunction, and incontinence. The video highlights the diagnostic process with MRI and lumbar puncture, and discusses treatment options such as high-dose corticosteroids, plasmapheresis, and long-term management with drugs like mycophenolate and rituximab. The goal is to provide a comprehensive understanding of transverse myelitis and its management.
Takeaways
- 😀 Transverse myelitis involves inflammation and demyelination of axons, particularly in the spinal cord, and its causes can be classified as peri-infectious, autoimmune, or idiopathic.
- 😀 Peri-infectious causes of transverse myelitis include viral infections like dengue and herpes, bacterial infections like mycoplasma pneumoniae, and parasitic infections like schistosomiasis.
- 😀 Autoimmune conditions such as multiple sclerosis and acute disseminating encephalomyelitis (ADEM) can also contribute to the development of transverse myelitis.
- 😀 The pathophysiology involves T cells crossing the blood-brain barrier, releasing cytokines (e.g., interleukin-1, interleukin-6, TNF-alpha), which trigger inflammation and damage to the spinal cord.
- 😀 Inflammation and immune responses in transverse myelitis can lead to increased vascular permeability, vasodilation, chemotaxis, and the recruitment of macrophages and other immune cells.
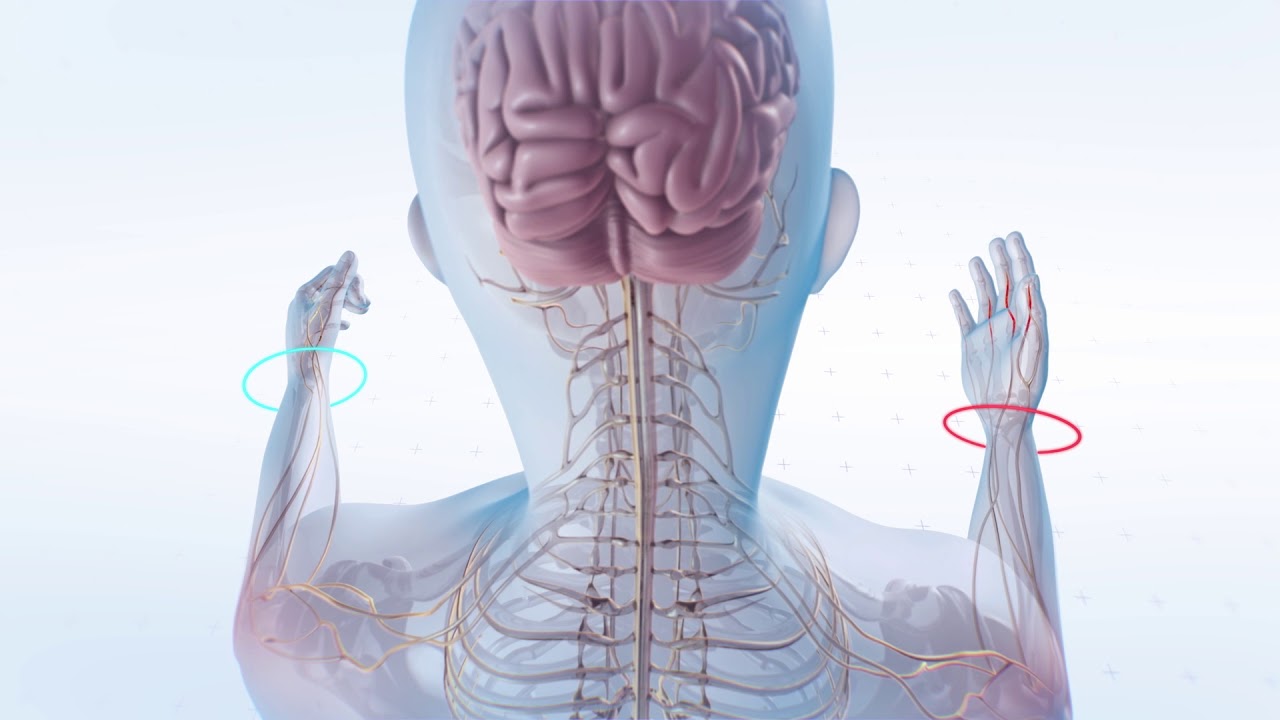
- 😀 The damage caused by transverse myelitis can result in demyelination and neuronal destruction, particularly in the thoracic region of the spinal cord, where it most commonly occurs.
- 😀 Clinical features of transverse myelitis include autonomic dysfunction (e.g., urinary and fecal incontinence), sensory deficits (e.g., loss of light touch, proprioception), and motor deficits (e.g., spasticity or flaccid paralysis).
- 😀 Depending on the affected spinal cord region, transverse myelitis can cause upper motor neuron signs (e.g., spasticity, hyperreflexia) or lower motor neuron signs (e.g., flaccid weakness, fasciculations).
- 😀 Diagnosis is typically made with MRI of the spinal cord (with and without contrast) and lumbar puncture to look for pleocytosis (increased white blood cells in CSF).
- 😀 Treatment options include high-dose corticosteroids as the first-line therapy, and second-line treatment with plasmapheresis if corticosteroids are ineffective or contraindicated. Long-term management may involve immunosuppressive drugs like mycophenolate or rituximab to control inflammation and prevent relapse.
Q & A
What is transverse myelitis?
-Transverse myelitis is an inflammatory condition that affects the spinal cord, leading to demyelination and potential axonal destruction. It is caused by a variety of factors, including infections, autoimmune diseases, and idiopathic reasons.
What are the primary causes of transverse myelitis?
-Transverse myelitis can be caused by infections (e.g., viruses like dengue and herpes, bacteria like Mycoplasma pneumoniae, and parasites like schistosomiasis), autoimmune diseases (e.g., multiple sclerosis and acute disseminating encephalomyelitis), and in some cases, the cause is idiopathic.
How does the pathophysiology of transverse myelitis lead to spinal cord damage?
-In transverse myelitis, immune system activation leads to inflammation of the spinal cord. T-cells, antibodies, and cytokines like IL-1, IL-6, TNF-alpha, and interferon-gamma contribute to the inflammatory process, which damages the myelin sheath and potentially destroys axons, disrupting normal neurological function.
What are the key clinical symptoms of transverse myelitis?
-The clinical features of transverse myelitis include sensory and motor deficits (e.g., weakness, sensory loss), autonomic dysfunction (e.g., urinary or fecal incontinence), and sometimes cerebellar involvement leading to ataxia. Symptoms vary depending on which part of the spinal cord is affected.
What is the role of MRI in diagnosing transverse myelitis?
-MRI of the spinal cord is crucial for diagnosing transverse myelitis. It shows hyperintense lesions on T2-weighted images, which indicate areas of inflammation. Contrast-enhanced MRI can highlight active lesions, which helps confirm the diagnosis.
What is the significance of lumbar puncture in the diagnosis of transverse myelitis?
-A lumbar puncture can show pleocytosis, which refers to an increased number of white blood cells, particularly T-cells and B-cells, in the cerebrospinal fluid. This suggests inflammation of the spinal cord, which is a key diagnostic feature of transverse myelitis.
What are the first-line and second-line treatments for transverse myelitis?
-First-line treatment for transverse myelitis includes high-dose corticosteroids, which help reduce inflammation. If corticosteroids are ineffective or contraindicated, plasmapheresis (a process that clears harmful proteins and antibodies) is used as a second-line treatment.
What are the long-term treatment options for transverse myelitis?
-Long-term management options for transverse myelitis include immunosuppressive medications like mycophenolate, which inhibits the production of inflammatory cytokines, and rituximab, which targets immune cells (T-cells, B-cells, and macrophages) to reduce inflammation and prevent recurrence.
What role does mycophenolate play in the treatment of transverse myelitis?
-Mycophenolate is an immunosuppressive drug that inhibits the production of cytokines such as interleukin-1, interleukin-6, and tumor necrosis factor alpha. This helps reduce the inflammation and immune response associated with transverse myelitis, potentially preventing relapse.
Why is rituximab considered an effective treatment for transverse myelitis?
-Rituximab works by inhibiting immune cells, including T-cells, B-cells, and macrophages, which are involved in the inflammatory process in transverse myelitis. Additionally, rituximab stimulates regulatory T-cells that have anti-inflammatory effects, helping to calm down the immune response and reduce further spinal cord damage.
Outlines

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنMindmap

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنKeywords

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنHighlights

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنTranscripts

هذا القسم متوفر فقط للمشتركين. يرجى الترقية للوصول إلى هذه الميزة.
قم بالترقية الآنتصفح المزيد من مقاطع الفيديو ذات الصلة

Trauma Medulla Spinalis (Part 1) - Anterior & Posterior Cord Syndrome, Transverse Lesion
Gray and white matter | Organ Systems | MCAT | Khan Academy

Sensory Pathways | Touch/Proprioception vs Pain/Temperature

Spinal Cord - Overview

Cerebrospinal Fluid (CSF) explained in 3 Minutes - Function, Composition, Circulation
What is Multiple Sclerosis? An Overview of MS Causes, Symptoms, Treatments & Research
5.0 / 5 (0 votes)
